Abstract
Background: Navigating difficult conversations is an expectation of Pediatric practitioners upon completion of graduate medical education (GME). Often however, clinical experience during residency does not, on its own, adequately prepare residents to confidently engage patients and families in difficult conversations. In addition, even when ample clinical opportunity is present, feedback regarding success and opportunities for improvement from colleagues and, in particular, families and patients on how a resident managed a difficult conversation may not be readily available.
Research Question: We sought to evaluate if a simulated patient (SP) workshop involving difficult conversations would improve resident comfort with difficult conversation scenarios while educating pediatric residents on specific communication tools, tenets from culturally effective healthcare and inter-professional team work in a peer-focused environment.
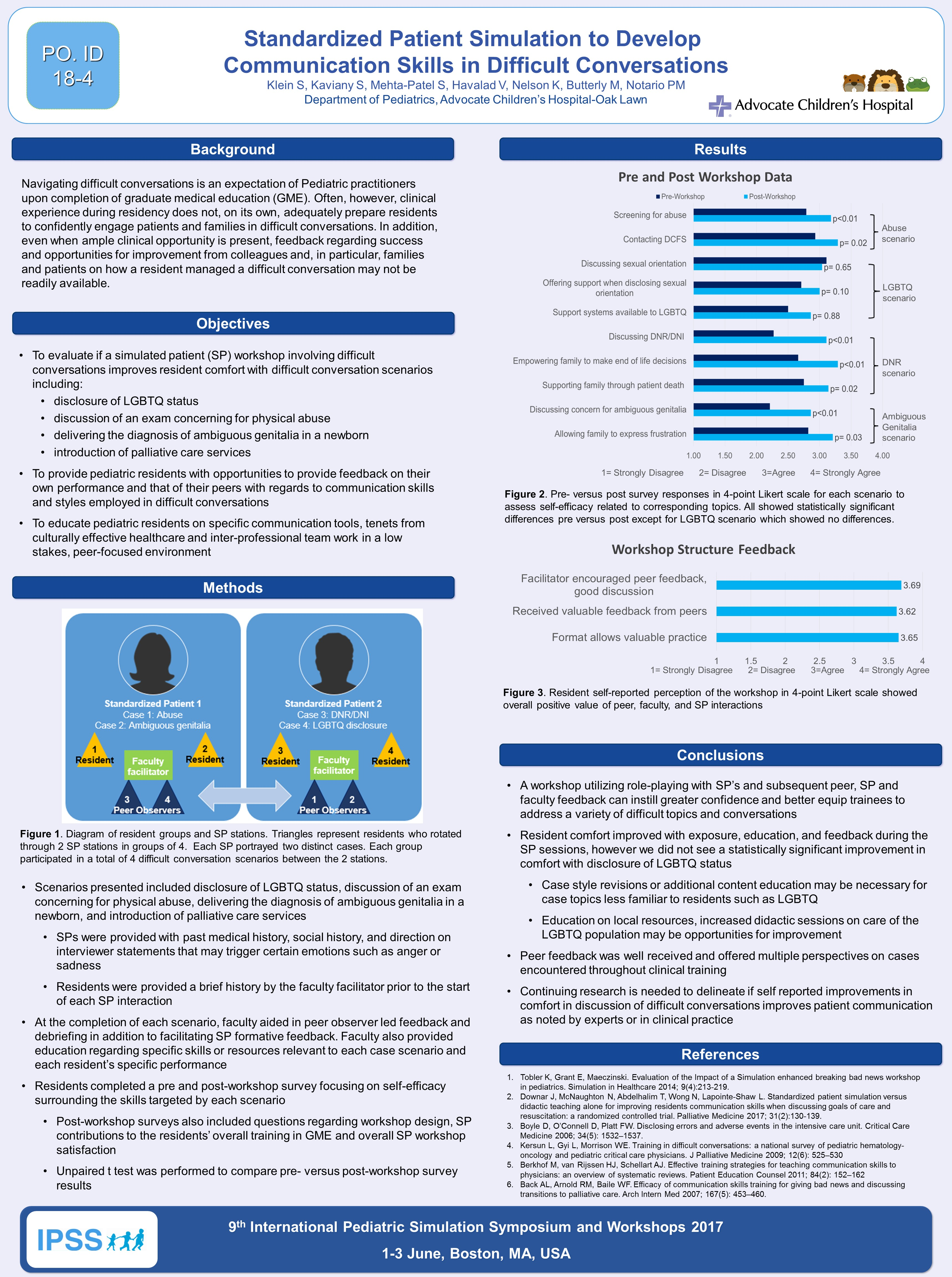
Methodology: Residents were divided into peer groups of four. These groups rotated through two SP stations. Each station consisted of one faculty supervisor and one SP trained on enacting two distinct difficult conversation scenarios. These scenarios included disclosure of LGBTQ status, discussion of an exam concerning for physical abuse, delivering the diagnosis of ambiguous genitalia in a newborn and introduction of palliative care services. Peers within the group and the group faculty facilitator observed an individual resident’s interaction with the SP caregiver. At the completion of each scenario, faculty provided formative, on-the-spot, feedback, and aided in peer observer led debriefing in addition to direct feedback from the SP. Faculty also provided education regarding specific skills or resources relevant to each case scenario and each resident’s specific performance. Residents completed a survey focusing on self-efficacy surrounding the skills targeted by the SP workshop both prior to the start of and following completion of the workshop. The post-workshop survey also included questions regarding workshop design, SP contributions to the residents’ overall training in GME and overall SP workshop satisfaction. Unpaired t test performed to compare pre- versus post-workshop surveys.
Results: Pre- versus post survey responses showed statistically significant increases (p>0.05) in comfort and confidence in engaging families for all cases except LGBTQ case. Resident self-reported perception of the workshop showed overall positive value of peer, faculty and SP interactions.
Discussion/Conclusions: A workshop utilizing role-playing with SP’s and subsequent peer, SP and faculty feedback can instill greater confidence and better equip our trainees to address a variety of difficult topics and conversations. Case style revisions or additional content education may be necessary for case topics less familiar to resident such as LGBTQ.