Abstract
Purpose:
Microsurgery and radiation treatment (RT) are therapeutic options for vestibular schwannomas (VS). Our purpose was to examine long-term outcomes in a geographically defined population of patients.
Materials and Methods:
This is a population-based, retrospective review of 342 patients treated for VS between 2002-2009, having a potential minimum follow-up of 5 years. Patient management was routinely chosen after discussion in a provincial multidisciplinary conference. The primary endpoint was local control and the secondary endpoint was treatment-related toxicity. Serviceable hearing (SH) was measured using the Gardner-Robertson scale and facial nerve dysfunction (FND) using the House-Brackmann (HB) grading. Progression free survival (PFS) was estimated using the Kaplan-Meier method. Serious adverse events (SAEs) were graded using the Common Terminology Criteria for Adverse Events (version 4.03).
Results
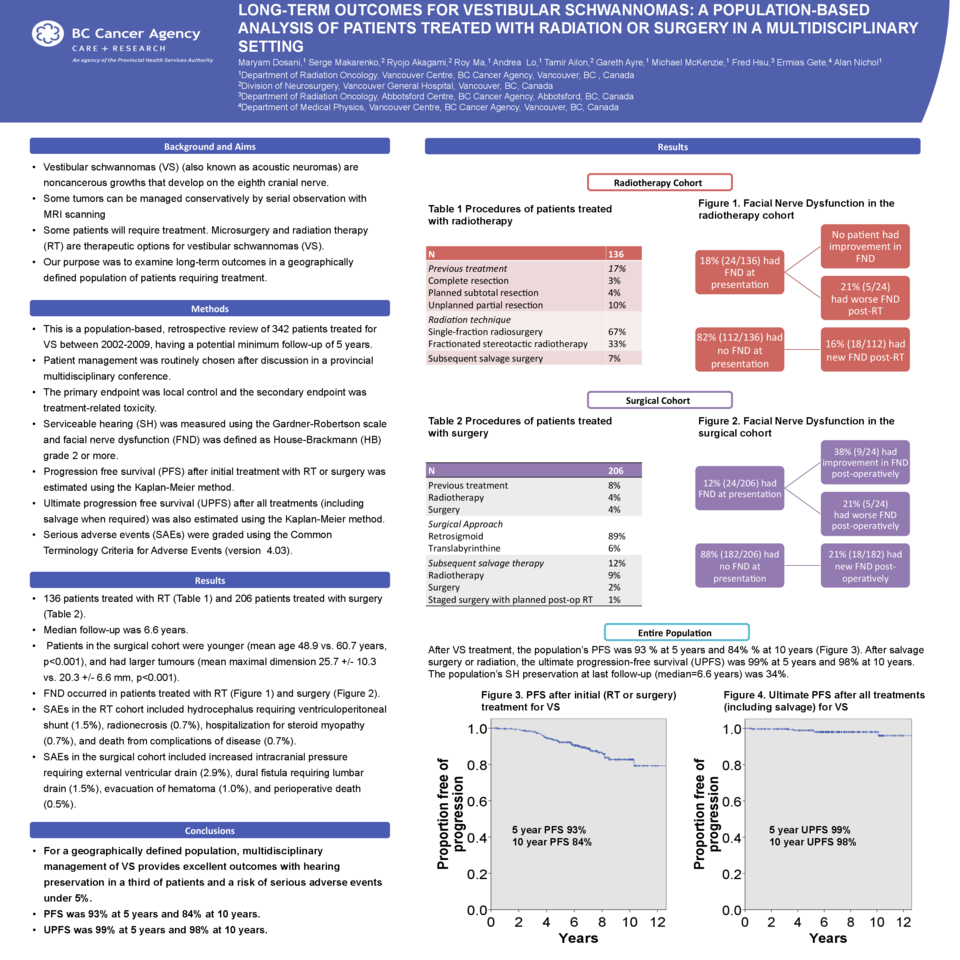
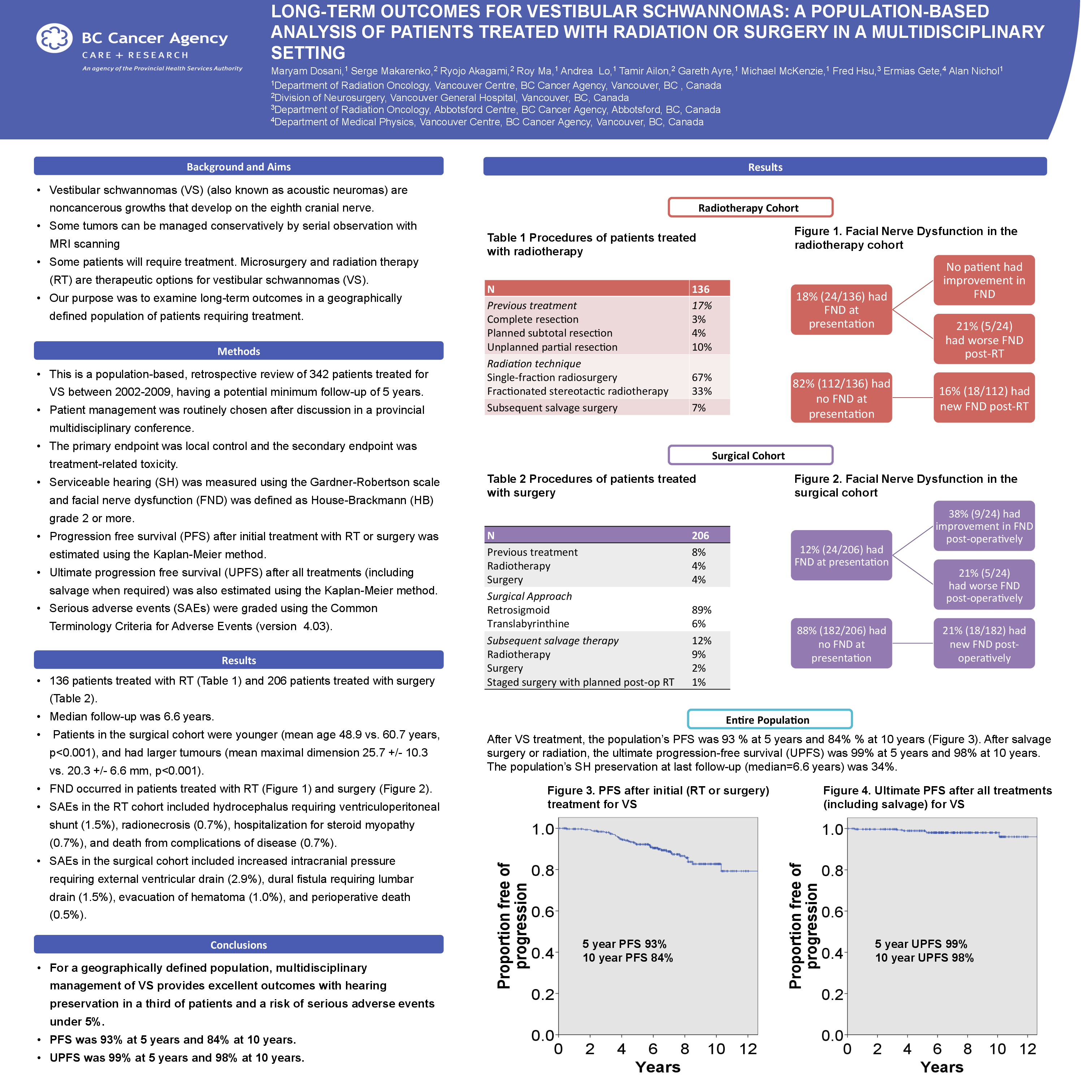
The study population consisted of 206 patients treated with surgery and 136 patients treated with RT. Median follow-up was 6.6 years. Patients in the surgical cohort were younger, with mean age: 48.9 vs. 60.7 years, p<0.001, and had larger tumours, with mean maximum dimension: 25.7 +/- 10.3 mm vs 20.3 +/- 6.6 mm, p<0.001.
After all VS treatments, the population’s PFS was 92.8 +/- 1.5% at 5 years and 83.7% +/- 2.9% at 10 years. The population’s SH preservation at last follow-up was 34.2%. SAEs occurred in 4.7% of patients.
In the radiotherapy cohort of 136 patients, 17% had previous surgery (4 complete resection, 5 planned subtotal resection and 14 unplanned partial resection). 67% had single-fraction stereotactic radiosurgery and 33% had fractionated stereotactic radiotherapy. 7% (10/136) had progressive disease requiring salvage surgery. 18% had FND (HB grade 2 or more) at presentation. No patients had improvement in FND after RT and 17% had new or worsened FND after treatment. SAEs were: hydrocephalus requiring ventriculoperitoneal shunt 1.5% radionecrosis 0.7%, hospitalization for steroid myopathy 0.7% and death from complications of disease 0.7%.
In the surgical cohort of 206 patients, 8% had previous treatment (8 radiation, 9 surgery). The most common surgical approaches were retrosigmoid (89%) and translabyrinthine (6%). 2% had planned post-op RT and 12% had disease progression requiring salvage: 19 RT, 3 surgery, 2 unknown. 12% had FND at presentation. FND improved in 4.4% and worsened in 12.6% after surgery. SAEs were: increased intracranial pressure requiring external ventricular drain 2.9%, dural fistula requiring lumbar drain 1.5%, evacuation of hematoma 1.0%, and perioperative death 0.5%.
Conclusion
Multidisciplinary management of VS provides excellent disease control at a population level with hearing preservation in a minority of patients and a low risk of serious adverse events.