Abstract
Purpose: Volumetric changes can be observed on serial cone-beam computed tomography (CBCT) images obtained throughout the course of radical radiotherapy for non-small cell lung cancer (NSCLC). This study aims to a) examine whether the magnitude of tumor regression is correlated with disease control and survival outcomes; b) explore the potential difference between adenocarcinoma and non-adenocarcinoma NSCLC subtypes.
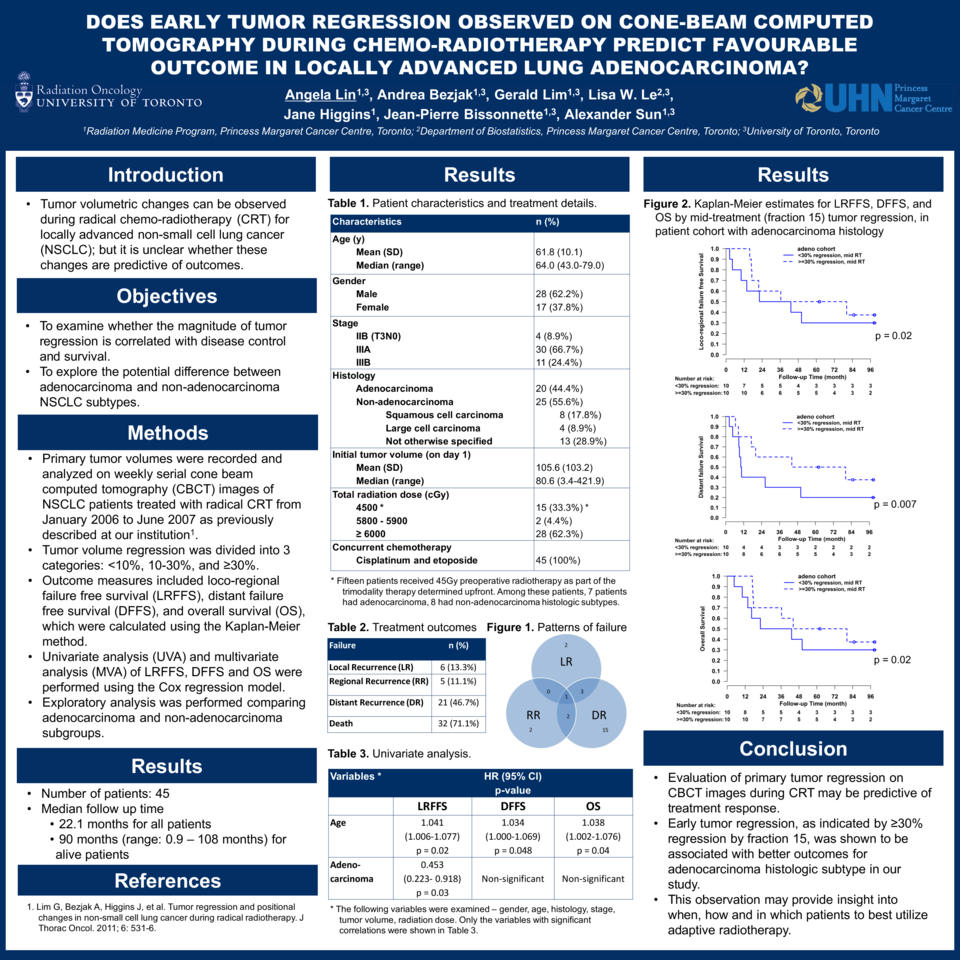
Materials and Methods: In a previous study from our institution, primary tumor volumes were recorded and analyzed on weekly serial CBCT images of 60 NSCLC patients treated with radical chemo-radiotherapy. We performed a retrospective review of these patients, and documented patient-, tumor-, and treatment-related details. Outcome measures included loco-regional failure free survival (LRFFS), distant failure free survival (DFFS), disease free survival (DFS) and overall survival (OS), which were calculated using Kaplan-Meier method. Univariable analysis (UVA) and multivariable analysis (MVA) of LRFFS, DFFS, DFS and OS were performed using Cox regression model. Further analysis was performed for the adenocarcinoma and non-adenocarcinoma subgroups.
Results: Forty-five patients with locally advanced NSCLC were included, after excluding 15 patients who had radical local radiotherapy for either oligometastatic stage IV disease or recurrent disease after initial surgical management. Median age was 64 years (range: 43 – 79 years). Median follow-up was 22.1 months for all patients, and 90 months for alive patients (range: 0.9-108 months). The distribution of 7th ed. AJCC stage was as follows: stage II 8.9%; IIIA 66.7%; IIIB 24.4%. Twenty patients (44.4%) had adenocarcinoma, while 25 patients (55.6%) had non-adenocarcinoma histologic subtypes. Twenty-eight patients (62.3%) received total radiation dose ≥ 60 Gy, 15 patients (33.3%) received 45 Gy as neoadjuvant therapy, and 2 patients (4.4%) received 58-59 Gy due to missed fractions. Among all 45 patients, 23 patients (51.1%) had more than 30% regression by fraction 15 and 32 patients (71.1%) by treatment completion. In UVA, adenocarcinoma (p=0.03) was associated with better LRFFS; young age was associated with better LRFFS (p=0.02), DFFS (p=0.048) and OS (p=0.04). In MVA, large regression by fraction 15 was associated with better DFS (p=0.047). For patients with adenocarcinoma, MVA showed that large regression by fraction 15 was associated with better DFFS (p=0.01), DFS (p=0.01) and OS (p=0.02). For patients with non-adenocarcinoma, larger regression by treatment completion and trimodality therapy (radiation dose of 45Gy) were associated with better LRFFS (p=0.02, 0.04).
Conclusions: Evaluation of tumor regression on CBCT images during radiotherapy may be predictive of treatment response. Early tumor regression, as indicated by regression ≥ 30% by fraction 15, was associated with better DFS for all patients; and early tumor regression was associated with better DFFS, DFS and OS for the adenocarcinoma cohort. This observation may provide insight into when and how to best utilize adaptive radiotherapy.