Abstract
Background and Purpose:
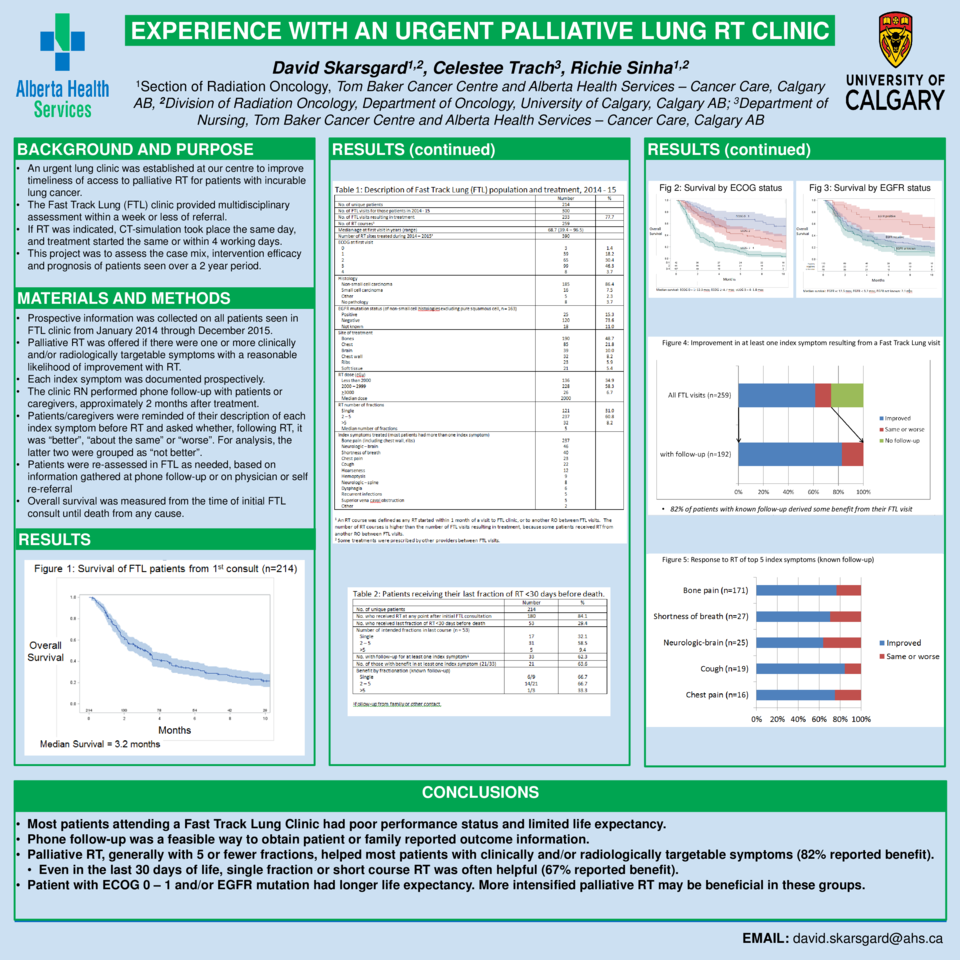
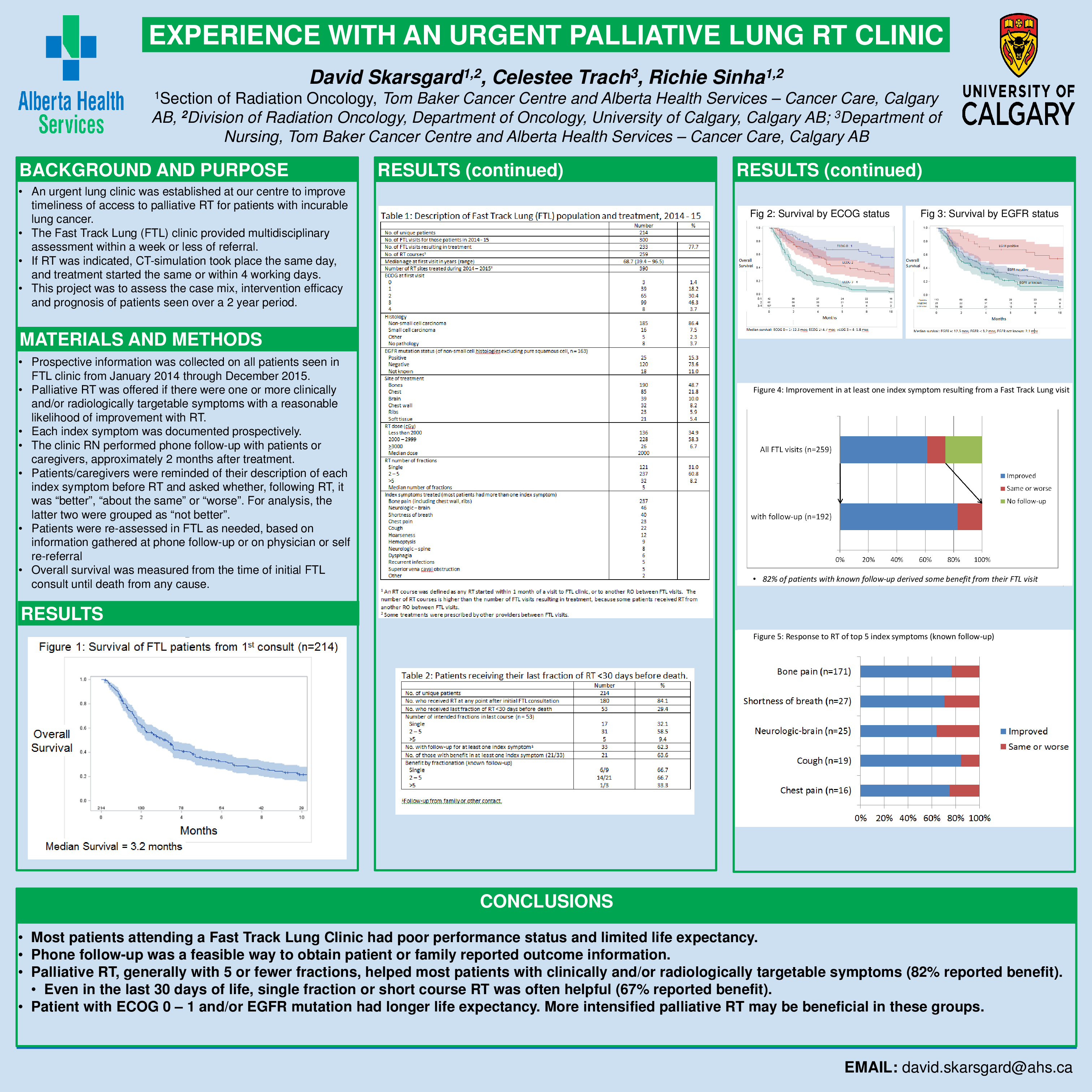
An urgent lung clinic was established to improve timeliness of access to palliative RT for patients with incurable lung cancer. The Fast Track Lung (FTL) clinic provides multidisciplinary assessment within a week of referral, followed by CT-simulation if appropriate, then treatment within 0 – 4 working days. This project was to assess the case mix, intervention efficacy and prognosis of patients seen over a 2 year period.
Materials and Methods:
Prospective information was collected on all FTL patients seen from Jan 2014 to Dec 2015. Palliative RT was offered if there were one or more clinically and/or radiologically targetable symptoms with a reasonable likelihood of improvement with RT. Phone follow-up by a nurse 1 – 2 months later assessed the effect of RT on each index symptom.
Results:
Two hundred fourteen patients were assessed a total of 300 times, a mean of 1.4 times per patient (range 1 – 8). 86% had non-small cell histologies (71% adenocarcinoma, 22% squamous cell carcinoma). Most were ECOG 2 (30%) or 3 (46%) at the time of first presentation. Median survival from initial FTL consult was 3.2 months (95% CI 2.2 – 3.6) for the entire group; for ECOG 0 – 1, it was 12.3 months (95% CI 7.4 – 16.2) and for ECOG 3 – 4, 1.8 months (95% CI 1.5 – 2.2). EGFR mutation positive patients had a median survival of 12.5 months (95% CI 4.3 – 39.8). There were 259 courses of RT to 390 sites, a mean of 1.5 per patient, range 0 – 13, and 192 of those courses (74%) had phone follow-up of at least one index symptom. 49% of RT courses were delivered to bony sites other than ribs, 22% to the chest, 14% to the chest wall/ribs and 10% to the brain. 31% were single fractions and 92% were < 5 fractions. Median dose was 20 Gy and the median number of fractions was 5. Among patients with follow-up information who received RT to one or more concurrent site(s), 82% reported benefit in at least one index symptom. This varied by symptom (e.g. cough 84%, bone pain 77%, shortness of breath 70%, hoarseness 40%). Even when the last fraction of RT was given within the last 30 days of life, an intended course of 5 or fewer fractions helped at least one index symptom in two-thirds of patients.
Conclusions:
Most patients attending FTL clinic had poor performance status and limited life expectancy. Phone follow-up was a feasible way to obtain patient or family reported outcome information. Palliative RT, generally with 5 or fewer fractions, helped most patients with clinically and/or radiologically targetable symptoms. Even within the last 30 days of life, single fraction or short course RT was often helpful. Patients with ECOG 0 – 1 and/or EGFR mutation had a longer life expectancy. More intensified palliative RT may be beneficial in these groups.