Abstract
Introduction
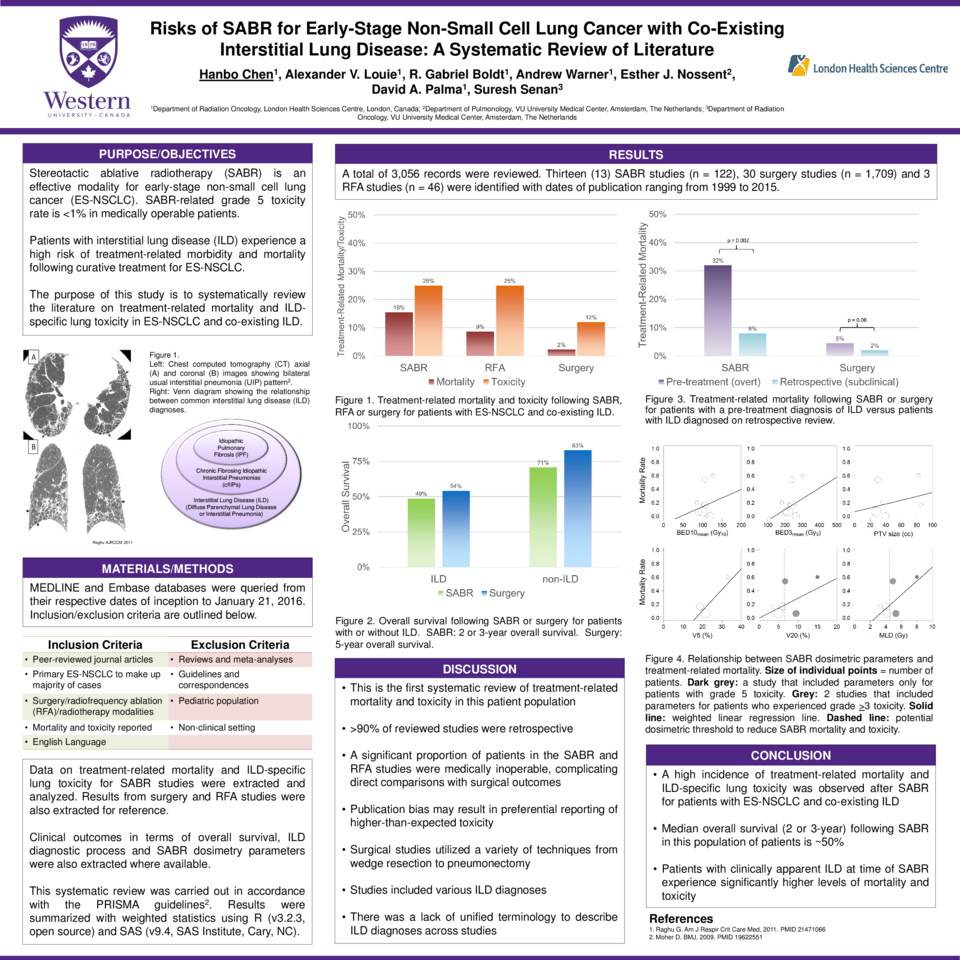
Treatment options for early-stage non-small cell lung cancer (ES-NSCLC) are generally well-tolerated. However, there has been an increasing number of reports where patients with interstitial lung disease (ILD) suffer severe toxicity after treatment for NSCLC. The purpose of this study was to explore treatment-related toxicity following curative ES-NSCLC treatment in patients with co-existing ILD, with a focus on potential factors that can identify patient groups at high versus low risk for toxicity.
Methods
A systematic review of literature was performed in accordance with PRISMA guidelines. The Medline and EMBASE databases were queried from respective dates of inception to January 2016. Treatment modalities included radiotherapy, surgery and radiofrequency ablation (RFA). Results were summarized with weighted statistics. Fisher’s exact test was used to calculate p-values.
Results
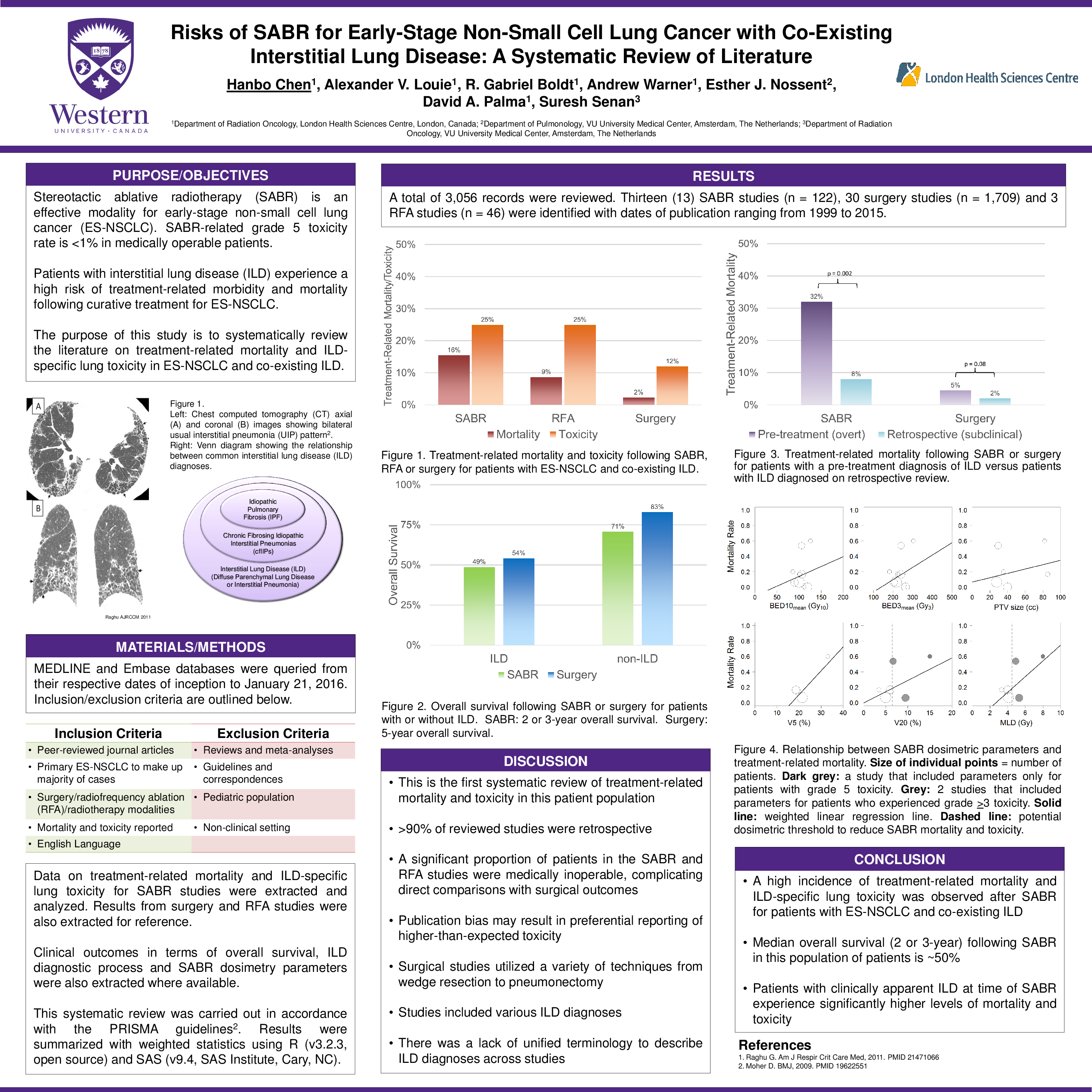
A total of 3,056 unique records were reviewed. Overall, 13 SABR studies (n = 122), 30 surgical studies (n = 1709), and 3 RFA studies (n = 46) were included. Most patients in non-surgical studies were medically inoperable. Treatment-related mortality was 15.5%, 8.7% and 2.3%, respectively, for SABR, surgery and RFA. Additionally, treatment-related acute exacerbation of ILD or radiation pneumonitis > grade 3 was 25%, 25% and 12%, respectively. For patients treated with SABR, median 2 to 3-year OS was 48.8% (range: 0%-53.8%) for patients with ILD and 70.8% (range: 54%-86.7%) for patients without ILD. For patients treated with surgery, median 5-year overall survival (OS) was 54.2% (range: 31.4%-61.6%) for patients with ILD and 83.0% (range: 70.5%-88.3%) for patients without ILD. For patients treated with SABR, subclinical ILD at time of treatment resulted in reduced mortality (p = 0.002) and toxicity (p = 0.004). Reduced mortality and toxicity was reported in SABR studies with V20 < 6.5% (p = 0.02 [mortality], p = 0.08 [toxicity]) or mean lung dose (MLD) < 4.5 Gy (p = 0.01 [mortality], p = 0.03 [toxicity]).
Conclusion
A high level of treatment-related toxicity is observed in patients treated for ES-NSCLC with co-existing ILD. Medically inoperable patients experienced high levels of treatment-related mortality. However, there is equipoise in overall survival after treatment with either SABR or surgery. Patients treated with SABR are at reduced risk for mortality and toxicity with V20 < 6.5%, MLD < 4.5 Gy or subclinical ILD at time of treatment.