Abstract
Purpose
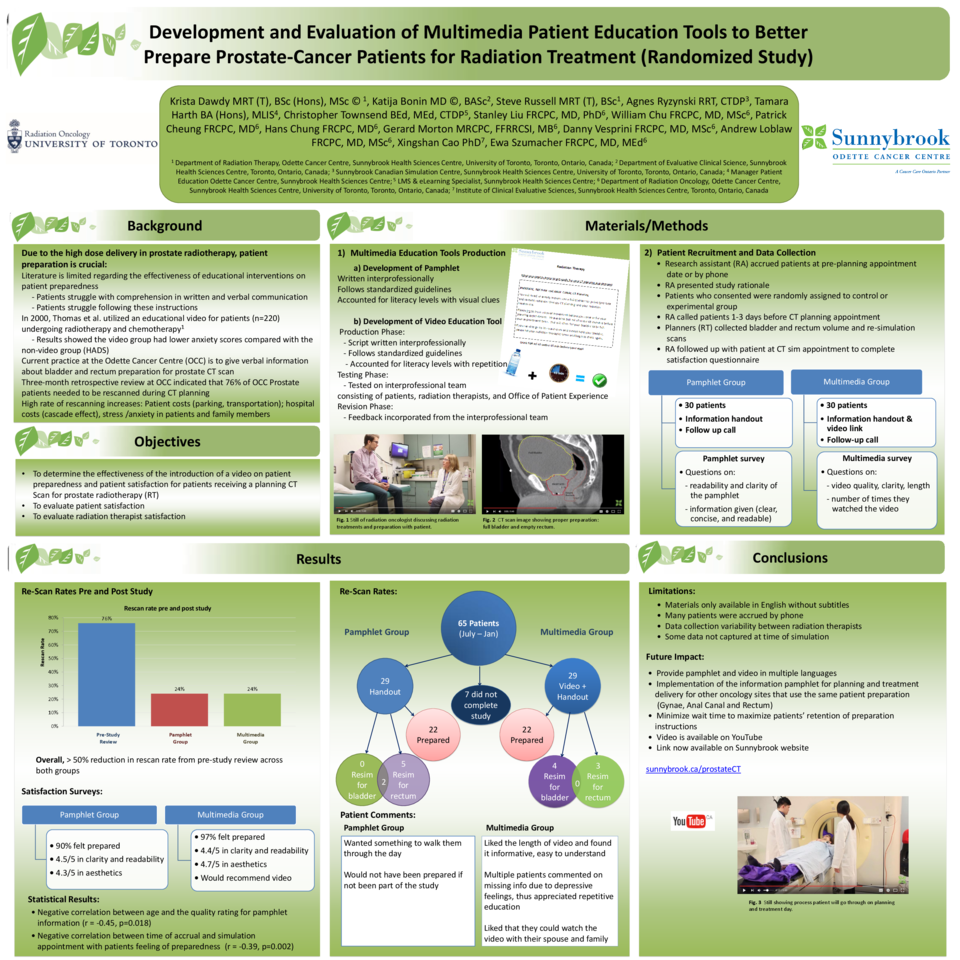
A review of patient preparedness for prostate radiotherapy (RT) showed that 13/55 patients were prepared and 42/55 (76%) needed to be re-scanned due to inadequate bladder or rectum filling. To decrease additional scans, associated costs and patient satisfaction, a video outlining proper preparation for prostate RT was created. The purpose of this study was to determine the effectiveness of a video versus an educational handout to improve CT planning preparation for prostate RT.
Methods
A video outlining the importance of rectal and bladder preparation was created and revised based on clinical feedback from an interprofessional team consisting of patients, radiation oncologists, nurses and radiation therapists. Patients were accrued by the research assistant (RA) in new patient clinics and randomly assigned to either the control group (received handout) or the experimental group (watched video and received handout). The RA followed up with patients at their planning CT simulation appointment to determine if patients were prepared or needed re-simulation and to evaluate patients’ satisfaction with the preparation materials (handout or video). A Likert scale was used to determine patient satisfaction outcomes.
Results
58/65 patients completed the study, with 29 patients in each arm. The mean age in the control group was 71 and 68 in the experimental group. In the control group, 23/29 were prepared for planning CT scan and 6/29 needed to be rescanned due to full rectum (5/28), empty bladder (0/28) or both (2/28), with one person needing to be rescanned twice. In the experimental group, 22/29 were prepared and 7/29 needed to be rescanned due to full rectum (4/28) or empty bladder (5/28), with two people needing to be rescanned twice. There was no statistical difference between groups in re-scanning rate. Most patients were planned within 11 days after consenting to the study. Patients in the experimental group watched the video 1.4 times on average and expressed feeling more prepared for their appointment than the control group. Patients indicated that they liked the length of the video and would recommend the video to other patients with prostate cancer.
Conclusion
The CT re-simulation rate was 55% lower in the control group and 52% lower in the experimental group compared to the initial review. Despite no statistical difference in re-simulation rates between the groups, patient satisfaction in the experimental group was higher.