Abstract
Purpose. Survival is often overestimated in a palliative care (PC) population, yet clinicians rely upon such predictions when recommending therapy and assisting patients in end of life decisions. We explored the accuracy of survival predictions among multidisciplinary team members who independently evaluated patients with advanced or metastatic cancer while providing usual clinical care.
Methods. Healthcare professionals (HCPs) from the palliative radiation oncology and PC services at our institution completed anonymous predictions of survival after clinical assessment of referred patients. Discipline of the assessor and factors influencing the estimate were also collected, along with abstraction of patient demographics, cancer type, and date of death. Summary statistics and Kaplan-Meier estimates of actual survival (AS) were obtained. Correlations between AS and clinical predictions of survival (CPS) were calculated using Spearman’s correlation coefficient (r).
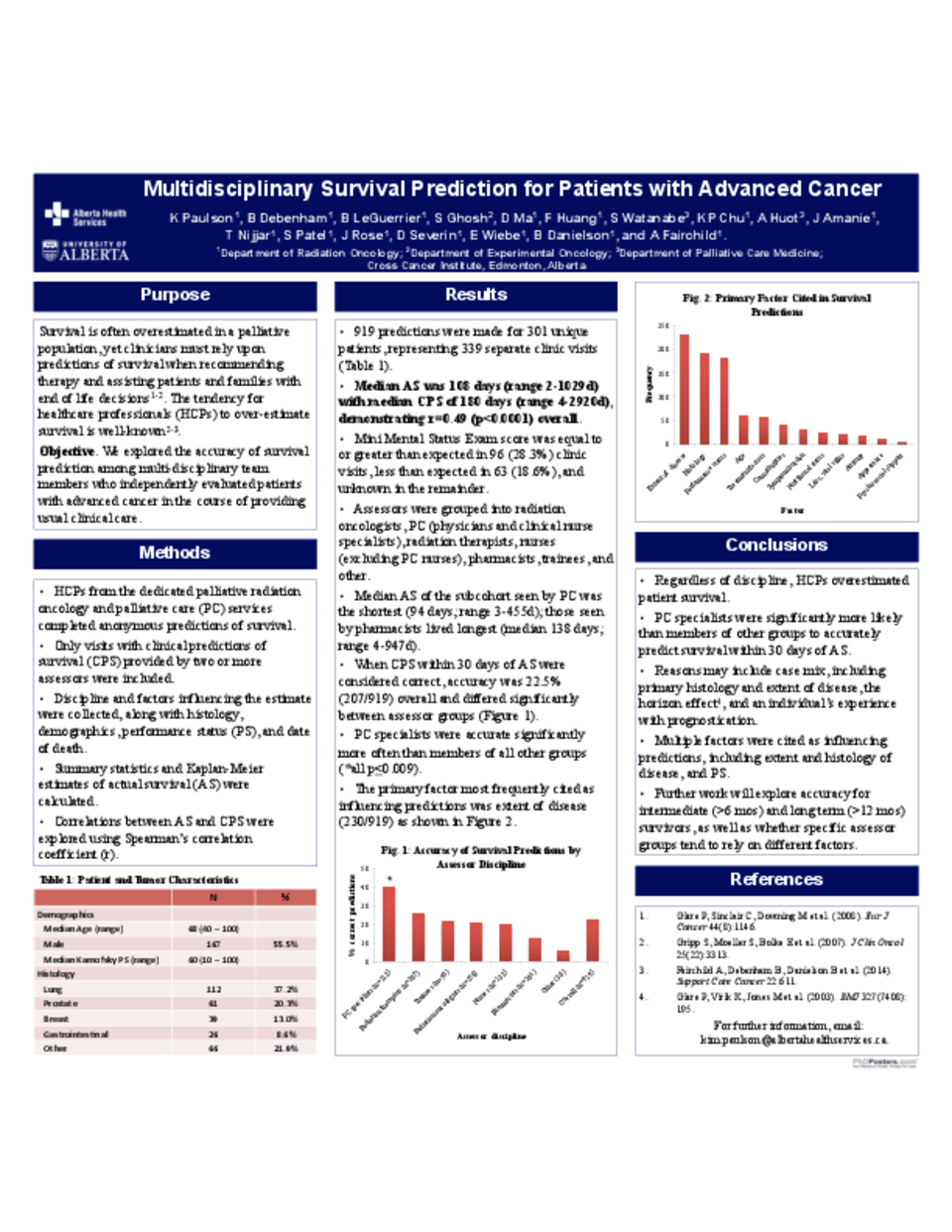
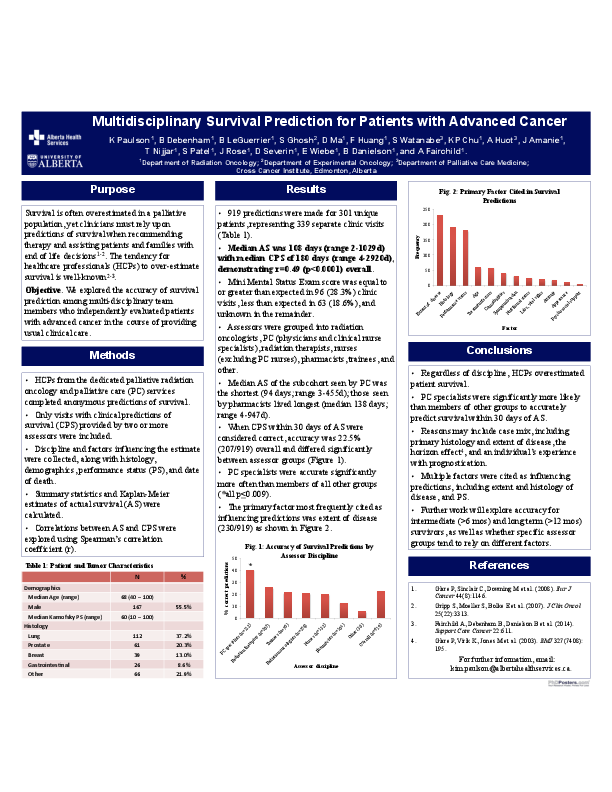
Results. 919 predictions were made for 301 unique patients (339 separate clinic visits). 55.5% were male, with a mean age of 67.8 years. 37.2% had lung cancer and 20.3% prostate cancer. Median AS was 108 days (range 2-1029d), and median CPS was 180 days (range 4-2920d), r=0.49 (p<0.0001). Median AS of the subcohort seen by the PC team was the shortest (94 days; range 3-455d); those seen by pharmacists lived longest (median 138 days; range 4-947d). When predictions within 30 days of AS were considered correct, accuracy was 22.5% (207/919) overall and 40.2% (45/112) for PC specialists (physicians and registered nurses [RNs]), 25.6% (53/207) for radiation therapists (RTTs), 21.4% (15/70) for trainees, 20.5% (53/258) for radiation oncologists, 19.7% (26/132) for nurses (RNs and nurse practitioners, excluding PC RNs), 12.5% (13/104) for pharmacists, and 5.6% (2/36) for other HCPs. PC specialists were accurate significantly more often than members of all other groups (all p<0.009). The primary factor cited was disease extent (230/919).
Conclusions. Regardless of discipline, HCPs overestimated survival; however, PC specialists were more likely to accurately predict survival to within 30 days of AS. Reasons may include case mix, including primary histology and extent of disease, the horizon effect, and individuals’ experience with prognostication. Future work will explore accuracy for intermediate (>6 months) and long term (>12 months) survivors.