Abstract
Nhu-Tram Nguyen1, Han Zhang2, D. Ian Hodson1, Lilian Doerwald-Munoz1, Jim Wright1
1Juravinski Cancer Centre, Hamilton, ON
2University of Alberta, Edmonton, AB
Purpose: Management of head and neck squamous cell carcinoma of unknown primary (HSCCUP) remains controversial. Many centres have adopted triple modality therapy with surgery followed by chemoradiation (S-CRT) as the preferred treatment method. However treatment regimens including: radiation (RT) and or chemotherapy (C) combined with or without surgery (S) used alone or in combination are still prevalent depending upon tumour and patient factors. Our study evaluated the outcomes of patients with biopsy-proven HSCCUP treated with S-CRT and chemoradiation (CRT) or surgery followed by radiation (S-RT).
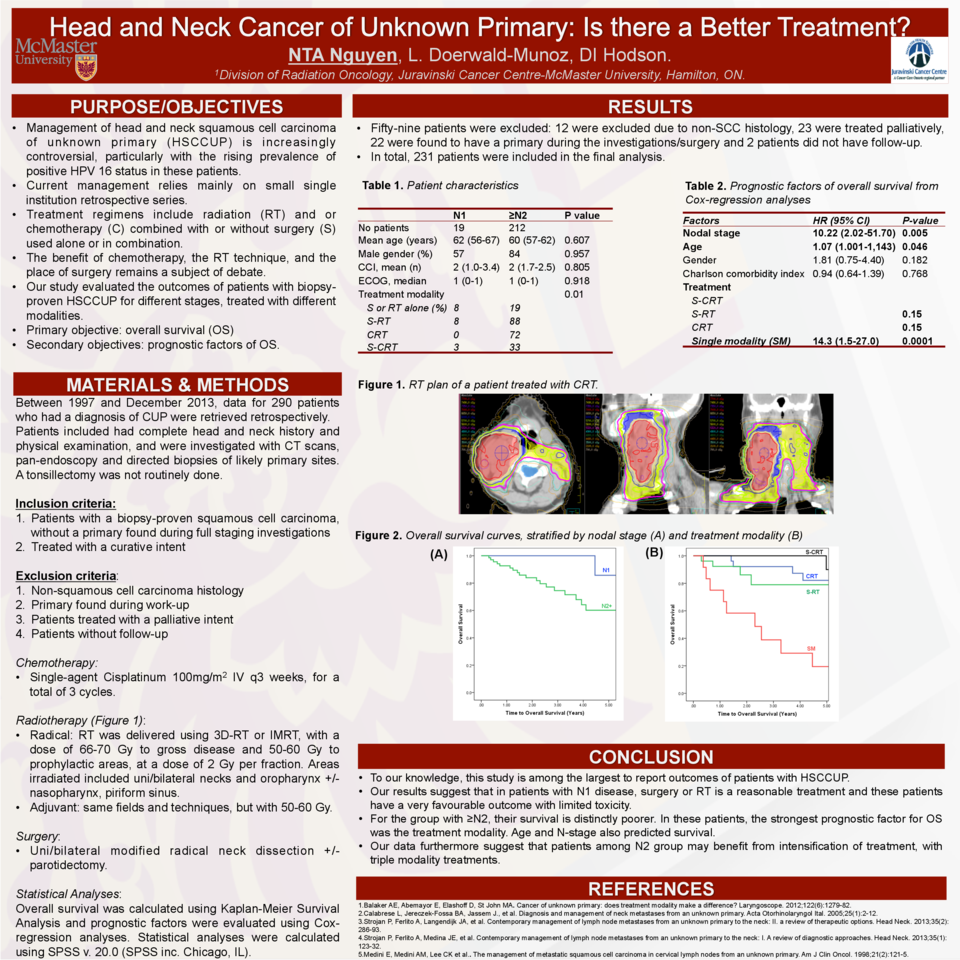
Materials and Methods: All patients with biopsy confirmed HSCCUP treated at the Juravinski Cancer Center (Hamilton, ON) with curative intent from 1998 to 2013 were included. Candidates for chemotherapy were administered with single agent Cisplatinum 100mg/m2 every three weeks, for a total of three cycles. Radiation (RT) fields included the nodal disease or surgical bed, the ipsilateral/bilateral neck as well as the oropharynx prophylactically. RT dose varied between 50 Gy to 70 Gy, depending on whether it was given as an adjuvant or primary treatment. The surgery involved most commonly a unilateral/bilateral neck dissection along with biopsies of high risk and suspicious areas for primary tumour. Demographic, pathological, outcomes and major toxicities were retrieved for all ,patients. Actuarial overall, disease specific and progression-free survivals were estimated using Kaplan-Meier method. Cox-regression analysis was also carried out with the co-variates set as age, gender, nodal staging, Eastern Cooperative Oncology Group performance scores (ECOG), and Charlson comorbidity index (CCI). Patients were grouped by treatment modalities.
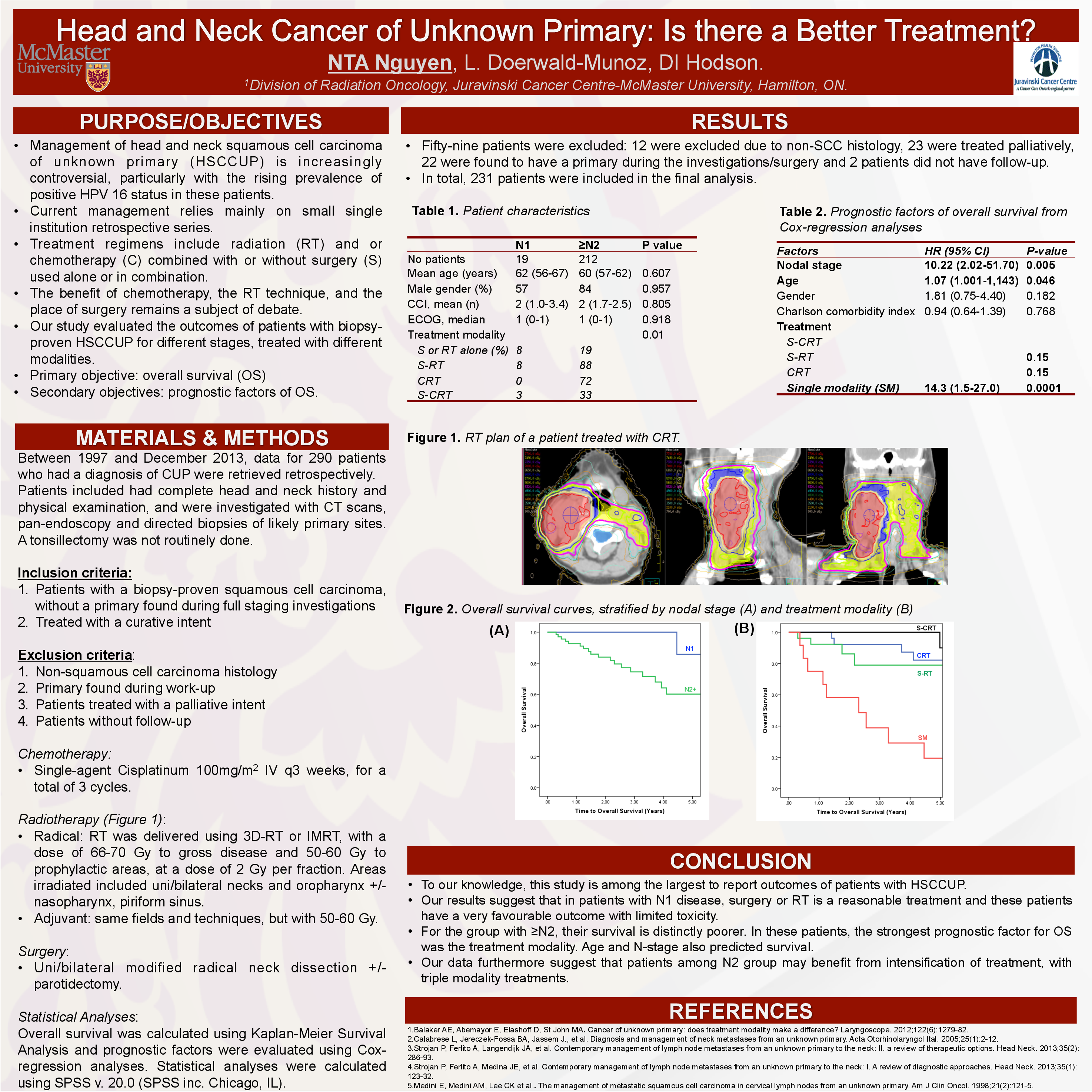
Results: A total of 210 patients were included. The median age was 60.2 years, median CCI-score was 2 and median ECOG was 1. Most patients had N2 (78%) and N3 (15%) disease, with only a minority presenting with N1 disease (6%). When divided into treatment groups, 26% were treated with S-RT, 49% with CRT, 19% with S-CRT; the remainder of patients were treated with single modality treatment such as RT alone/surgery alone. The five-year OS was to be 43% for the S-CRT group, 55% for the S-RT group and 74% for the CRT group. Comparative statistics showed lower nodal staging, lower CCI score, and treatment with S-CRT to be associated with statistically significant overall as well as progression-free survival benefits (p<0.05).
Conclusions: To our knowledge, this study is among the largest to report outcomes of patients with HSCCUP. Our results demonstrate that in patients with higher nodal stages, S-CRT was associated with better outcomes, with acceptable toxicities.