Abstract
Background:
Tracheostomies in infants and children are associated with significant risks of mortality and morbidity, most commonly tube obstruction and accidental dislodgment. Tracheostomy education is an essential part of pre-discharge planning in children with new tracheostomies. High-fidelity simulation has been shown to augment education for hospital staff.1 Proper education has the potential to decrease out-of-hospital events. Self-efficacy is a person’s context-specific sense of confidence in his or her ability to perform a particular behavior.2 Self-efficacy can be a proxy for competence because it has been show to directly correlate with performance.3 Evaluation of a caregivers’ preparedness for discharge is a common challenge for providers. A well-validated tool to measure caregivers’ competence is critical to determining readiness for discharge. It allows the measuring of effectiveness of a discharge educational program including high-fidelity simulation.
Research Question:
Develop and validate a tool measuring parental self-efficacy in caring for children with tracheostomies.
Methodology:
We created six domains of tracheostomy education and care based on four psychological processes of self-efficacy.
Using the modified Delphi method, content experts representing critical care, neonatology, psychology, family advocacy, and clinical nurse education winnowed questions over multiple rounds to establish content validity. Parent Advocates with tracheostomy care experience were then used to confirm content validity. The preliminary tool was comprised of 26 questions over six domains, and was administered to parents of children with a new tracheostomy and to experienced parents (children with tracheostomies >6 months) to determine response process.
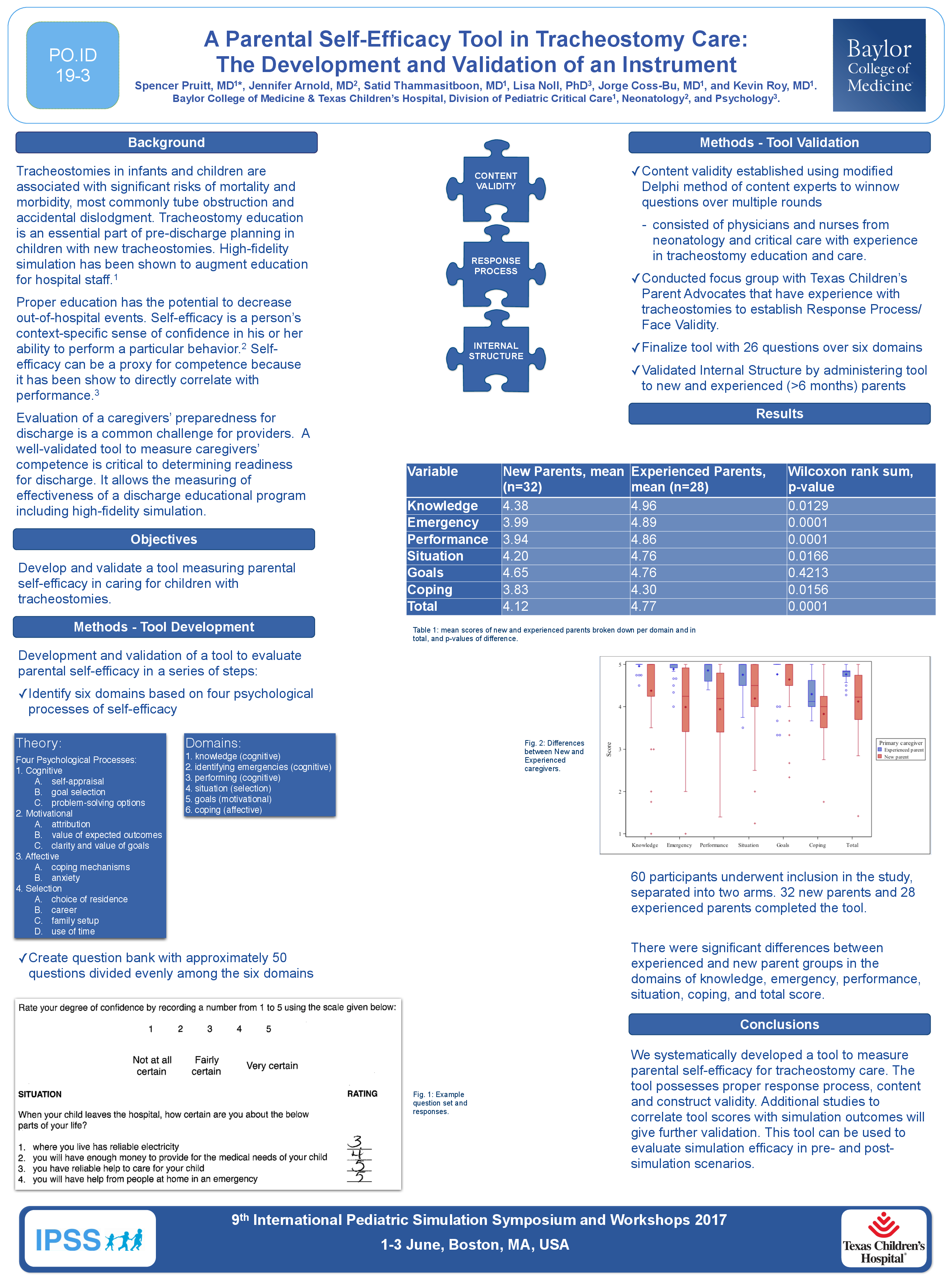
Subdomain scores were computed as the average of all responses to the questions within each subdomain and were then compared between experienced and new parents using the Wilcoxon rank sum test.
Results:
Sixty participants underwent inclusion in the study, separated into two arms. 32 new parents and 28 experienced parents completed the tool.
There were significant differences between experienced and new parent groups in the domains of knowledge, emergency, performance, situation, coping, and total score. The p-values were 0.0129, 0.0001, 0.0001, 0.0166, 0.0156, and 0.0001, respectively. The score on "Goals" was not significantly different (p=0.4213).
Conclusion:
We systematically developed a tool to measure parental self-efficacy for tracheostomy care. The tool possesses proper response process, content and construct validity. Additional studies to correlate tool scores with simulation outcomes will give further validation. This tool can be used to evaluate simulation efficacy in pre- and post-simulation scenarios.
References:
- Amit Agarwal, et al., “Improving Knowledge, Technical Skills, and Confidence Among Pediatric Health Care Providers in Management of Chronic Tracheostomy Using a Simulation Model,” Pediatric Pulmonology. 2016; 51:696-704.
- Albert Bandura, “Self-Efficacy: The Exercise of Control,” W.H. Freeman & Co: New York, 1997.
- Jennifer Plant, et al., “Validation of a self-efficacy instrument and its relationship to performance of crisis resource management skills,” Advances in Health Science Education. 2011; 16:579-590.