Abstract
Context: Chronic health conditions affect 7-18% of US children, and are often accompanied by complex medical management1, which can result in families feeling overwhelmed and stressed.2 Traditional methods for educating and training families have largely been limited to discussion with clinicians and observation/practice with patients. While such teaching is necessary in preparing families to care for their child, this often proves insufficient to achieve full and successful knowledge/skill transfer.3
Through realistic opportunities to repetitively practice new skills in low-risk settings, simulation applied to patients and caregivers, offers unique methodologies and new paradigms (more aligned with the adult learner), which may improve knowledge acquisition and performance of technical skills,4 as well as reduce anxiety through increased perception of preparedness to function in emergency situations.5 Simulation for families may be particularly useful at the time of a new diagnosis, initiation of new therapies or technology, or prior to a procedure, as many families report feeling technically incompetent, anxious, and lacking in self-confidence when faced with novel medical experiences.2 Importantly, despite these potential benefits, simulation with families remains an underutilized tool infrequently discussed in the literature.2,6-8
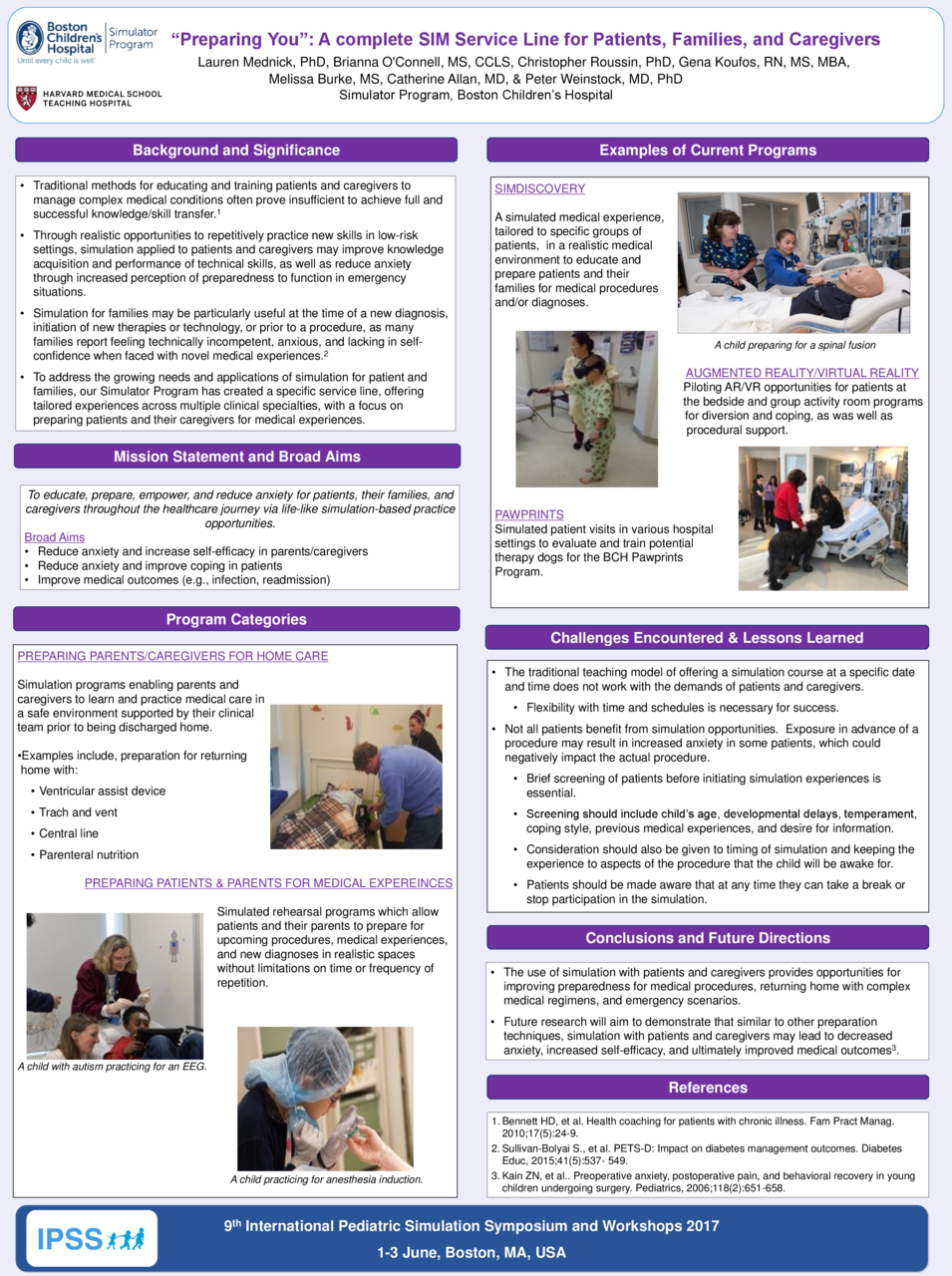
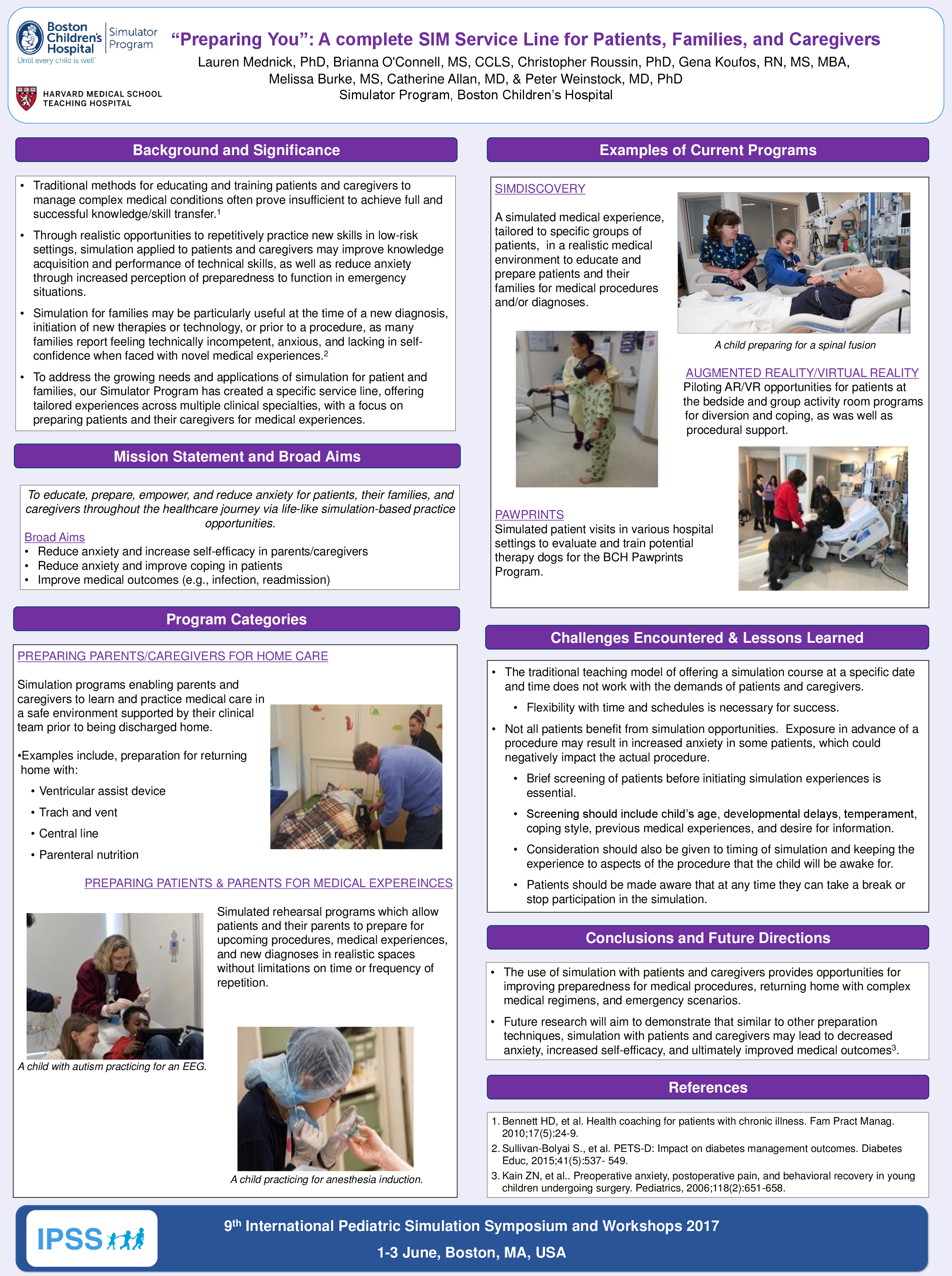
Description: To address the growing needs and applications of simulation for patient and families, our Simulator Program adapted all SOP to develop tailored experiences across multiple clinical specialties, culminating in a specific service line. To date, the service line has successfully initiated 6 projects, all at varying stages of completion. Current projects include simulation experiences targeted to families caring for a child with a vent and trach, patients and families returning home with a ventricular assist device, and patients preparing for invasive procedures such as an EEG or MRI.
The current presentation aims to discuss the construction, stages, and components of a “Preparing You” service line, benefits for both families and clinicians, and challenges encountered.
Observation/Evaluation: The authors will present pilot data demonstrating the impact of using simulation with families. Ultimately, as found with other preparation techniques, it is likely that decreased anxiety, increased self-efficacy, and improved cooperation achieved through simulation, could lead to improved medical outcomes.9
Discussion: The use of simulation with healthcare professionals is commonplace and benefits to clinicians and patients have consistently been demonstrated.4 A dedicated simulation service line specifically for patients and families, spins the tool 180 degrees, with the goal of improving the entire healthcare journey through an enhanced sense of preparation, support, and comfort. On-going work aims to further explore the benefits, as well as challenges, of this extension of traditional medical simulation.
References:
-
Perrin JM, Bloom SR, Gortmaker SL. The increase of childhood chronic conditions in the United States. . 2007;(24):2755-2759. PubMed PMID: .
-
Sullivan-Bolyai S, Crawford S, Bova C, Lee M, Quintos JB, Johnson K, Cullen K, Hamm T, Bisordi J, Ramchandani N, Fletcher J, Quinn D, Jaffarian C, Lipman T, Melkus G. PETS-D: Impact on diabetes management outcomes. Diabetes Educ, 2015;41(5):537-549. PubMed PMID: 26246593.
-
Bennett HD, Coleman EA, Parry C, Bodenheimer T, Chen EH. Health coaching for patients with chronic illness. Fam Pract Manag. 2010;17(5):24-9. PubMed PMID: 1121566.
-
Cook DA, Hatala R, Brydges R, Zendejas B, Szostek JH, Wang AT, Erwin PJ, Hamstra SJ. Technology-enhanced simulation for health professions education: a systematic review and meta-analysis. JAMA. 2011;306(9):978-988. PubMed PMID: 21900138.
-
Allan CK, Thiagarajan RR, Beke D, Imprescia A, Kappus LJ, Garden A, Hayes G, Laussen PC, Bacha E, Weinstock PH. Simulation-based training delivered directly to the pediatric cardiac intensive care unit engenders preparedness, comfort, and decreased anxiety among multidisciplinary resuscitation teams. J Thorac Cardiovasc Surg. 2010;140(3):646-652. PubMed PMID: 20570292.
- NM, Rutledge C, Zinkan JL, Youngblood AQ, Stone J, Peterson DT, Slayton D, Makris C, Magruder T, White ML. Ventilator caregiver education through the use of high- fidelity pediatric simulators: A pilot study. Clin Pediatr. 2013;52(11):1038-1043. PubMed PMID: 24137039.
Dracup K, Moser DK, Doering LV, Guzy PM, Juarbe T. A controlled trial of cardiopulmonary resuscitation training for ethnically diverse parents of infants at high risk for cardiopulmonary arrest. Crit Care Med. 2000;28(9):3289-3295. PubMed PMID: 11008994.
-
Ramchandani N, Maguire LL, Stern K, Quintos JB, Lee M, Sullivan-Bolyai S. PETS-D (parents education through simulation-diabetes): Parents' qualitative results. Patient Educ Couns. 2016;99(8):1362-1367. PubMed PMID: 27021779.
- ZN, Mayes LC, Caldwell-Andrews AA, Karas DE, McClain BC. Preoperative anxiety, postoperative pain, and behavioral recovery in young children undergoing surgery. Pediatrics, 2006;118(2):651-658. PubMed PMID: 16882820.