Abstract
Background
Many procedures identified by the Accreditation Counsel for Graduate Medical Education as essential to the practice of pediatric emergency medicine (PEM) are rarely performed by PEM physicians .1 Physicians feel that their opportunities for procedural practice are inadequate.2 There are currently no procedural training or procedural competency guidelines for PEM attendings.
Research Questions
What are current practices for providing procedural training and competency assessment for U.S. and Canadian PEM attendings?
Methods
Web-based survey to members of the PEM Fellowship Directors and Associate Fellowship Directors listserv, representing 91 PEM programs.
Results
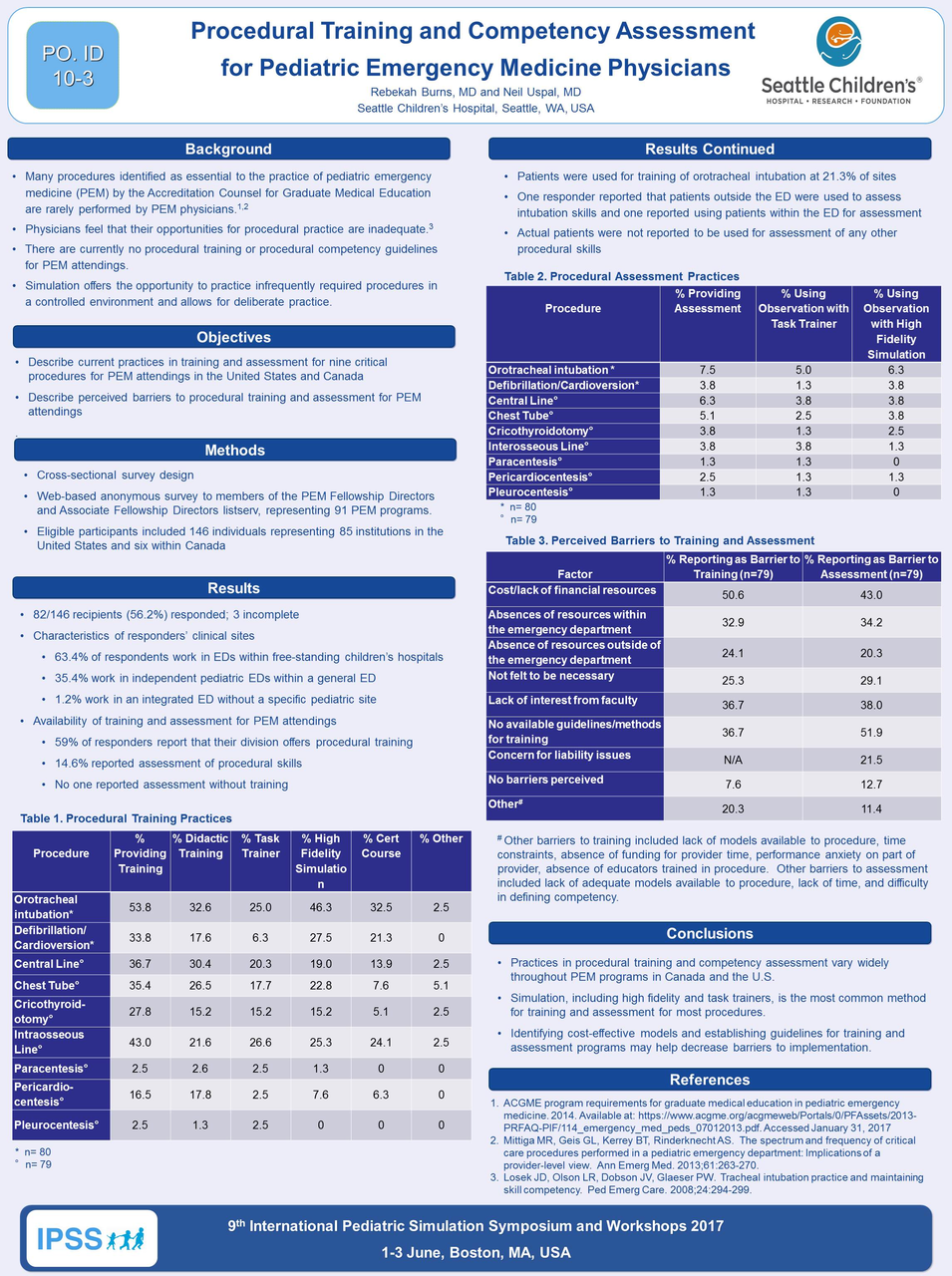
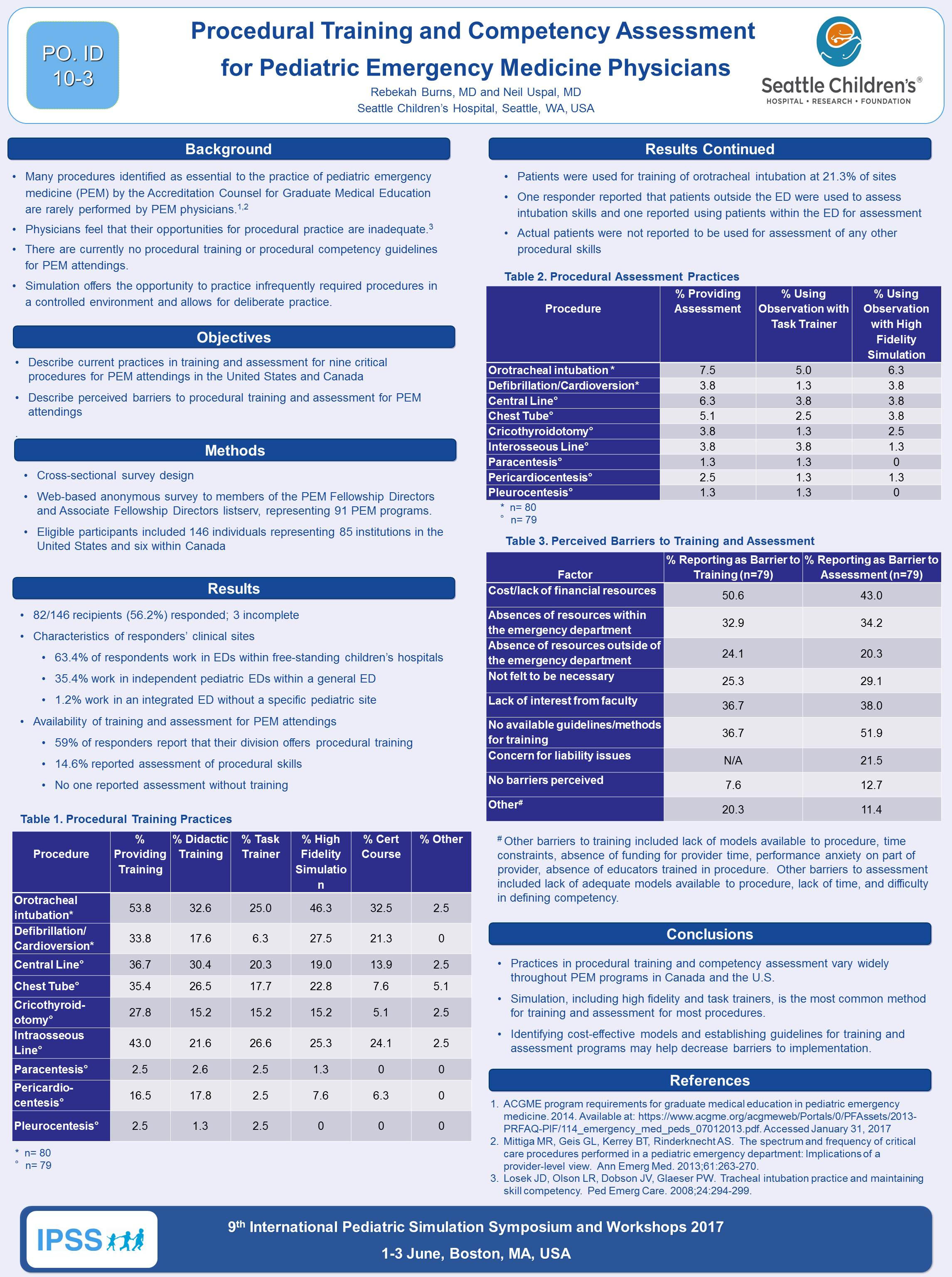
82 of 146 recipients (56.2%) responded. Three did not provide data on specific procedures. 63.4% of respondents work in EDs in free-standing Children’s Hospitals. 64.6% are part of a Department of Pediatrics. 58.5% of responders report that their divisions offer procedural training to attendings while 14.6% report assessment of procedural skills. No one reported assessment without training. The most common procedure for which training and assessment are offered are orotracheal intubation (53.4% and 7.5%, respectively) with high fidelity simulation being the most common method for both (37/43 and 5/6, respectively). Frequencies of training for other procedures include: Intraosseous line placement (43%), central line placement (36.7%), chest tube placement (35.4%), defibrillation/cardioversion (33.8%), cricothyroidotomy (27.8%), pericardiocentesis (16.5%), paracentesis (2.5%), pleurocentesis (2.5%). High fidelity simulation and task trainers are the two most common methods reported for training of all procedures except intubation (high fidelity and certification course), defibrillation/cardioversion (high fidelity and certification course), pericardiocentesis (lecture and high fidelity), pleurocentesis (task trainer and lecture). High fidelity simulation and task trainers are the most common methods of assessment for all procedures. 50.6% identify cost as a barrier to training with lack of faculty interest and lack of standardized guidelines the next most common barriers (36.4% each). Lack of standardized guidelines is the most common barrier for assessment (51.9%) followed by cost (43%) and lack of faculty interest (38%).
Discussion
Practices in procedural training and competency assessment vary widely throughout PEM programs in Canada and the U.S. Simulation, including high fidelity and task trainers, is the most common methods for training and assessment for most procedures. Identifying cost-effective models and establishing guidelines for training and assessment programs may help decrease barriers to implementation.
References
-
Mittiga MR, Geis GL, Kerrey BT, Rinderknecht AS.The spectrum and frequency of critical acre proceduers performed in a pediatric emergency department: Implications of a provider-level view.Ann Emerg Med. 2013;61:263-270.
-
Losek JD, Olson LR, Dobson JV, Glaeser PW. Tracheal intubation practice and maintaining skill competency. Ped Emerg Care. 2008;24:294-299.