Abstract
Purpose. Whole brain radiotherapy (WBRT) reduces neurological symptoms, increases median survival (MS), and remains a standard therapeutic modality for multiple brain metastases. Despite treatment, approximately half of patients will experience intracranial progression, for which repeat whole brain irradiation (ReRT) may be considered. While ReRT dose >20Gy may be associated with improved MS, there is no standard dosefractionation in use. This international collaboration investigated if dose correlates with OS.
Materials/Methods. Pooled (5 centers) database analysis included patients with multiple brain metastases from any solid primary tumor receiving 2 courses of WBRT. Patients treated with stereotactic radiosurgery or partial cranial RT were excluded. Demographics, disease characteristics, and RT doses were collected. Descriptive statistics were calculated, along with Spearman correlation coefficients (Rho) comparing Karnofsky performance status (KPS) and dose. MS was assessed using the Kaplan-Meier method and compared using the log-rank test. Cox regression analysis compared dose fractionation schedules.
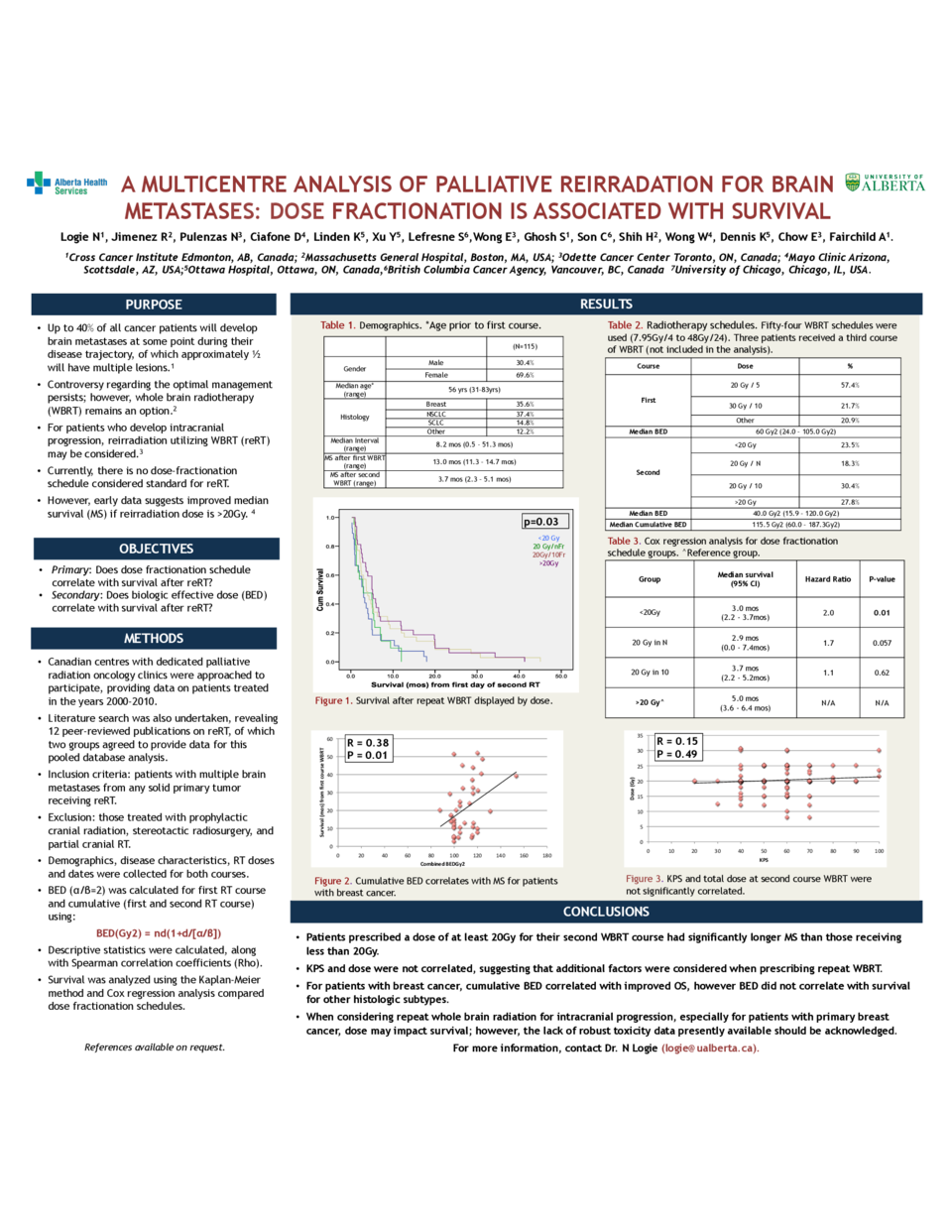
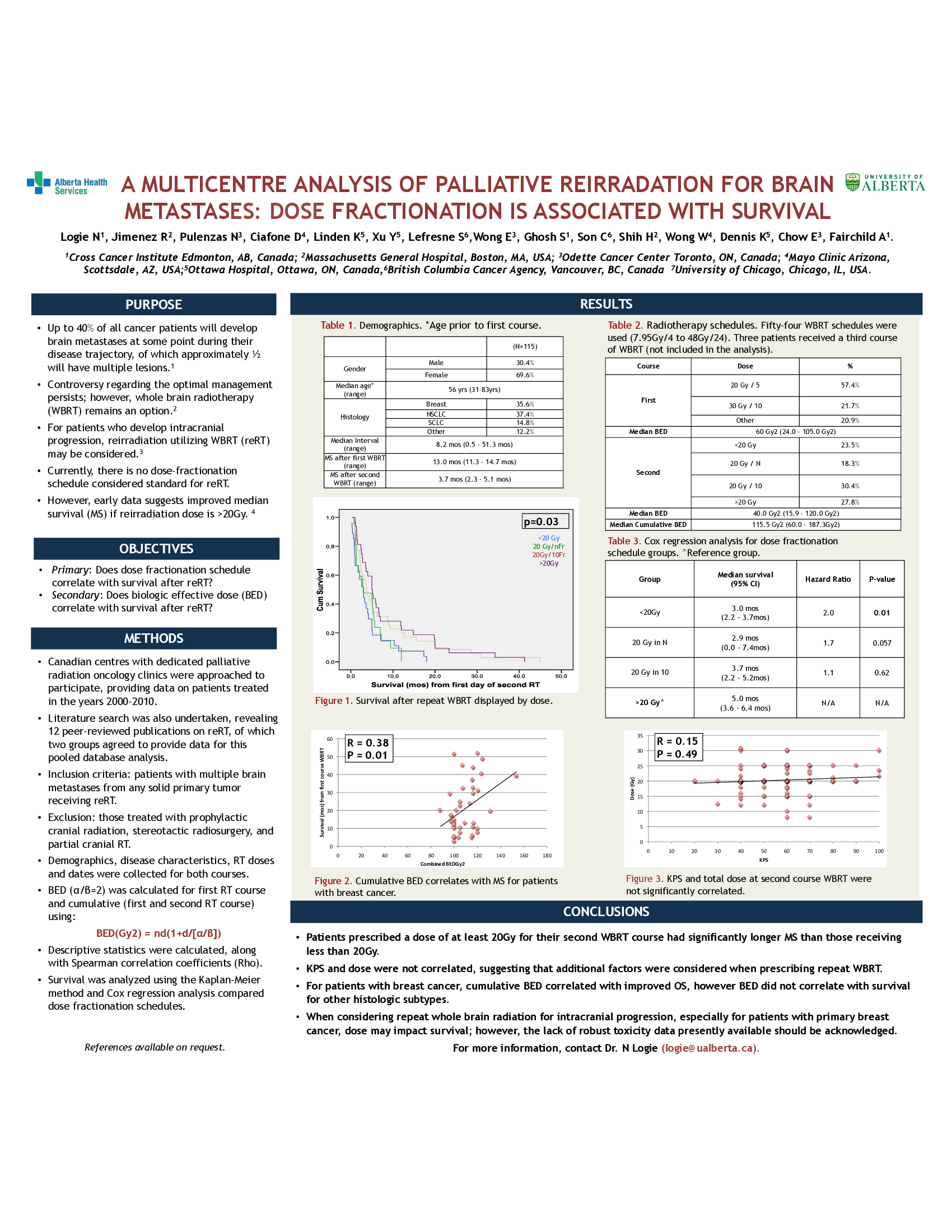
Results. One hundred fifteen patients met inclusion criteria: median age at first course (RT1) was 56 years, 69.6% (80/115) were female, 52.2% with lung and 35.7% breast cancer. Fifty-four WBRT schedules were used (range 7.95Gy/4 to 48Gy/24). Median interval between courses was 8.2 months (range 0.5 to 51.3 mos). For RT1, 57.5% received 20Gy/5. During the second RT course (RT2), 30.4% received 20Gy/10 while 27.8% received >20Gy. MS from first day of treatment for RT1 was 13.0 mos (95%CI 11.3-14.7 mos), and from first day of RT2 was 3.7 mos (95%CI 2.3-5.1 mos). Dosefractionation schedule significantly correlated with MS after RT2 (p=0.03). MS was highest for patients receiving >20Gy at RT2 (5.0 mos, 95% CI 3.6-6.4 mos) compared to <20Gy (3.0 mos, 95% CI 2.2-3.7mos), p= 0.01, hazard ratio=1.99. KPS and total dose at second course WBRT were not significantly correlated (Rho=0.15, p=0.11). Conclusions. Patients receiving >20Gy ReRT demonstrated an absolute improvement in
MS survival of 2 months compared to those receiving <20Gy. KPS and dose were not significantly correlated, suggesting that additional factors are taken into account when prescribing repeat WBRT. For eligible patients whose goal is maximal survival, >20Gy at the time of ReRT should be considered, acknowledging the lack of robust toxicity data presently available.