Abstract
Alexandra Waters, Guila Delouya, David Donath, Carole Lambert, Sandra Larrivée, Daniel Taussky
Université de Montréal, Montreal, QC
Purpose: PSA bounce (PSAb) following radiotherapy for prostate cancer is common in occurrence, yet its etiology remains unclear. There is contradiction and lack of validation in the literature as to its risk factors. This study aims to explore risk factors for a PSAb and determine its clinical significance.
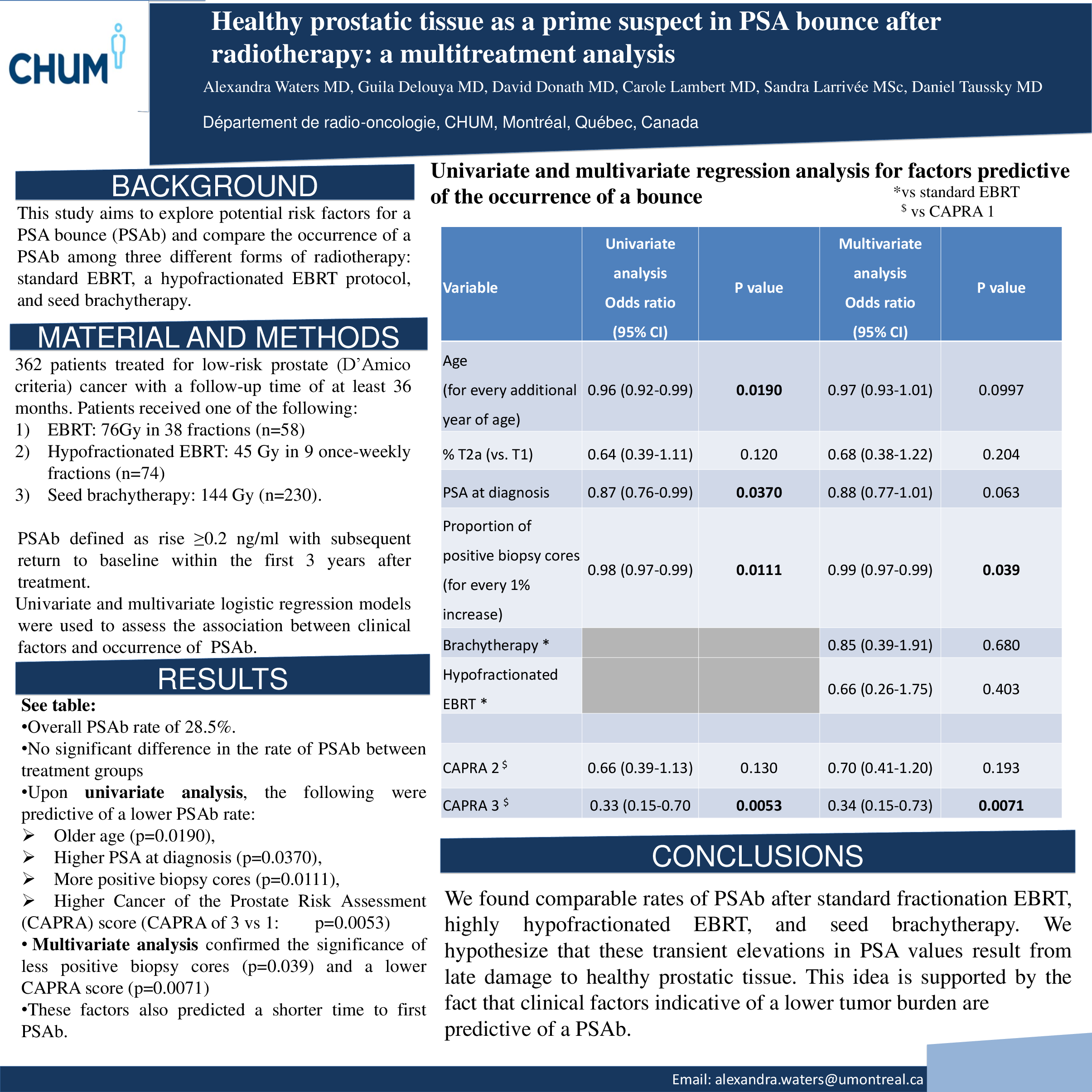
Materials and Methods: We identified 362 patients treated for low-risk prostate adenocarcinoma with a follow-up time of at least 36 months. Low risk was defined as PSA lower than 10 ng/ml, Gleason 6 or less, and clinical Stage T1a-T2a. Patients were treated with one of the following: 1) EBRT 76Gy in 38 fractions (n=58) 2) hypofractionated EBRT, 45 Gy in 9 once-weekly fractions (n=74) 3) LDR brachytherapy, prescribed dose 144 Gy (n=230). No patient received androgen deprivation therapy. PSA data was collected retrospectively. Post-treatment monitoring consisted of a serum PSA monitoring every 3 to 4 months for the first year, and biannually thereafter. The primary endpoint was the occurrence of a PSAb, which was defined as a rise of more than 0.2 ng/ml with subsequent return to baseline within the first 3 years after treatment. Univariate and multivariate logistic models were used to assess the association between clinical factors and occurrence of PSAb.
Results: There was no significant difference (p=0.083) between treatment groups, with an overall PSAb rate of 28.5%. No correlation between the occurrence of a PSAb and biochemical failure could be drawn, as only six failures occurred in the follow-up period. Upon univariate analysis, the following factors were found to be predictive of a lower PSAb occurrence: older age (OR=0.95, 95% CI 0.92-0.99, p=0.019), higher PSA at diagnosis (OR=0.87, 95% CI 0.76-0.99, p=0.037), more positive biopsy cores (OR=0.19, 95% CI 0.50-0.66, p=0.0054), and a higher Cancer of the Prostate Risk Assessment (CAPRA) score, which accounts for PSA level, Gleason score, clinical stage, percentage of positive biopsy cores, and age (CAPRA of 3 versus 1: OR=0.40, 95% CI 0.16-0.70, p=0.0053). Multivariate analysis showed that more positive biopsy cores (OR=0.25, 95% CI 0.064-0.90, p=0.039) was correlated to a lower rate PSAb. A separate multivariate model demonstrated that a lower CAPRA score was associated with a higher risk of PSAb (CAPRA 3 versus 1: OR=0.40, 95% CI 0.15-0.73, p=0.019). An alternate analysis was performed to identify factors associated with a shorter interval before PSAb. Models showed that the factors which correlated with a higher rate of PSAb also predicted a shorter interval between treatment and the occurrence of a PSAb.
Conclusions: We found comparable rates of PSAb after standard fractionation EBRT, hypofractionated EBRT, and LDR brachytherapy. We hypothesize that these transient elevations in PSA values result from late damage to healthy prostatic tissue. This idea is supported by the fact that clinical factors indicative of a lower tumour burden are predictive of a PSAb.