Abstract
G Rodrigues, S Senan, C Oberije, K Tsujino, T Wiersma, M Moreno-Jimenez, TH Kim, L Marks, R Rengan, L De Petris, S Ramella, K De Ruyck, N Rodrigues de Dios, A Warner, J Bradley, D Palma
Purpose: The clinical benefits/risks of dose escalation for stage III NSCLC remain uncertain despite results of the RTOG 0617 randomized trial. There is heterogeneity of practice with many clinicians prescribing intermediate levels of dose escalation between the 0617 study arms of 60 and 74 Gy. The recently released ASTRO guideline suggests a lack of evidence for this approach. This study investigated whether or not this strategy is associated with any survival benefits/risks by analyzing a large multi-institutional database of Stage III NSCLC patients treated with a variety of radiotherapy doses with concurrent chemoradiation.
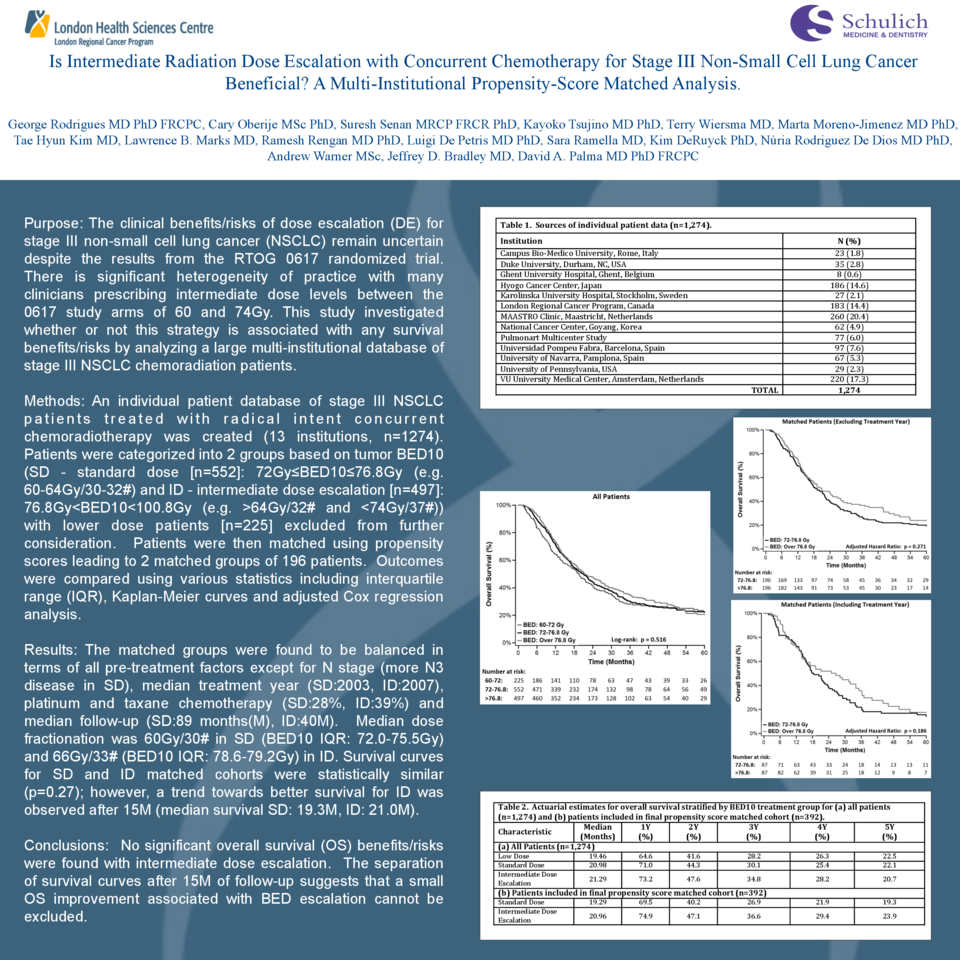
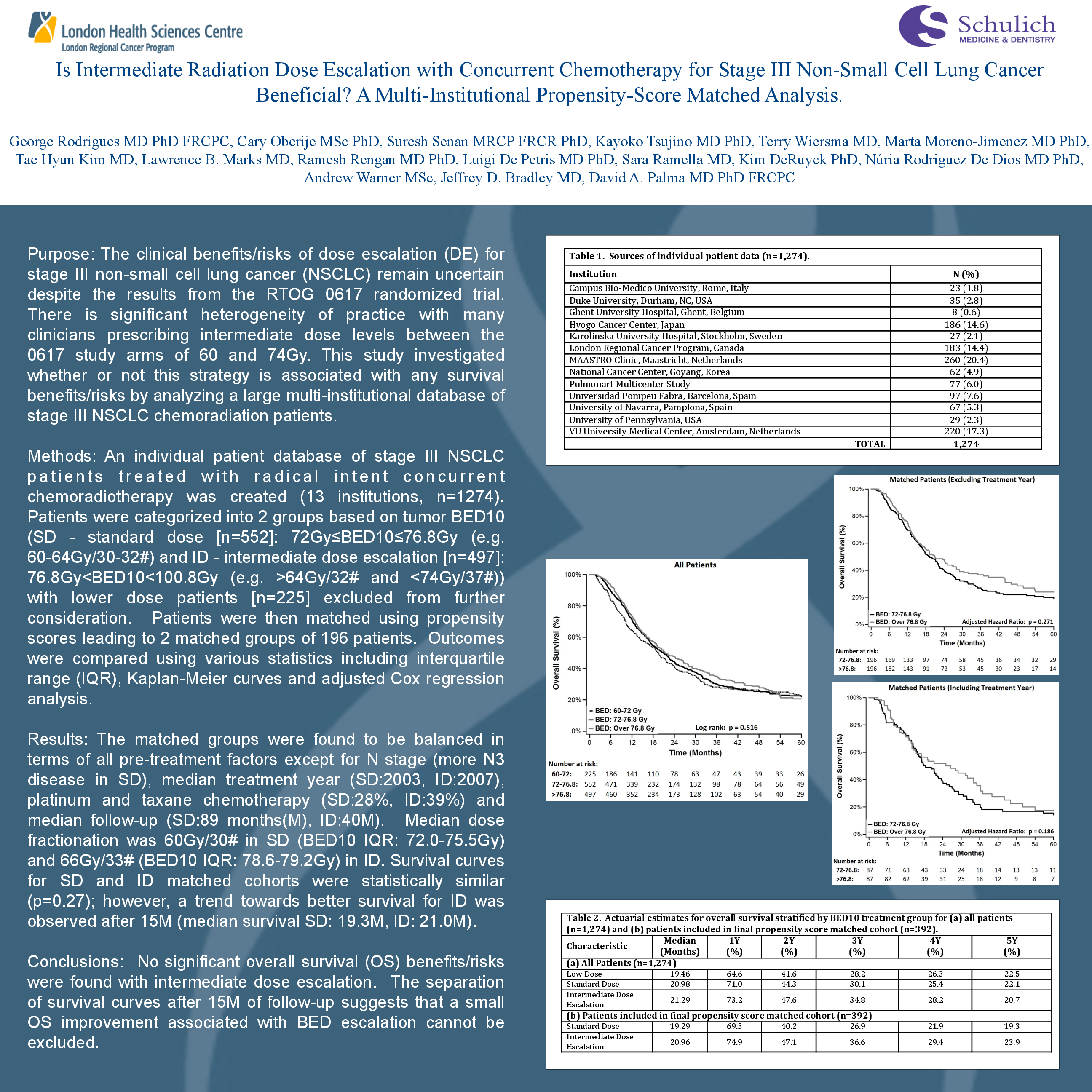
Materials and Methods: A multi-institutional individual patient database of Stage III NSCLC patients treated with radical concurrent chemoradiotherapy was created (12 institutions, n=1177). Patients treated with less than 60Gy/30# (biologically equivalent dose 10 – BED10 < 72 Gy) were excluded (n=197). Patients were categorized into two groups based on tumour BED10 (SD - standard dose [n=552]: 72Gy≤BED10≤76.8 Gy and ID - intermediate dose escalation [n=428]: BED10>76.8 Gy). Patients were matched using propensity scores based on sex, age, T-stage, tumour location, histology, and treatment year (1:1 match, caliper 0.10) leading to two matched groups of 196 patients. Descriptive statistics including interquartile range (IQR), Kaplan-meier curves and adjusted Cox p values were calculated to compare matched/unmatched groups.
Results: The groups were balanced in terms of all factors except for N stage (more N3 disease in SD), treatment year (median year, SD:2003 and ID:2008), platinum+taxane chemotherapy (SD:28%, ID:42%) and median follow-up (SD:90.6M, ID:34.7M). Median dose fractionation was 60 Gy/30# in SD (BED10 IQR 72.0-74.4 Gy) and 66 Gy/33# (BED10 IQR 78.0-79.2 Gy) in ID. Survival curves for SD and ID unmatched cohorts were statistically similar (p=0.98) with observed median survival of 20.5M and 19.4M, respectively. Survival curves for SD and ID matched cohorts were also statistically similar (p=0.11); however, a trend towards better survival for ID was observed after 12M. Median survival of SD and ID matched groups was 18M and 24M, respectively.
Conclusions: No significant overall survival (OS) benefits/risks were found with intermediate dose escalation in this analysis. The separation of survival curves after one year of follow-up suggests that optimal local control of disease may yet lead to small clinical improvements in OS.