Abstract
Introduction/Purpose
6 months androgen deprivation therapy (ADT) improves prostate cancer survival in Gleason 7 Prostate Cancer when added to conventional dose radiation (XRT) (D’Amico, JCO)1. The benefits of ADT when used in combination with dose escalated XRT remains to be determined. The purpose of the report is to evaluate the compliance, toxicity and efficacy of Dose Escalated XRT in combination with 6 months ADT (Zoladex + Casodex) in a Phase 3 Trial. The primary endpoint in the trial is to determine the optimal timing of XRT in relation to ADT.
Methods
438 patients were entered on the multi-center Phase 3 trial evaluating the optimal timing of Radical Radiation in combination with 6 months ADT.
Group A – ADT starts 4 months prior to radiation therapy
Group B – ADT starts Day 1 of radiation therapy
Inclusion criteria
cT1-T3, GL < 8, PSA < 30. Low risk prostate cancer patients were excluded.
Radiotherapy
6 Field 3DCRT/Fiducial based IGRT PTV1 56 Gy/28 PTV2 20 Gy/10
CTV1 = prostate + seminal vesicles CTV2 = prostate only PTV1 = CTV1 + 10mm except post 7mm PTV2 = CTV2 + 10mm except post 5mm
Primary Endpoint
PSA Disease Free Survival (PSA DFS)
Secondary Endpoints
Overall Survival (OS), Local Control (LC), Toxicity, QOL
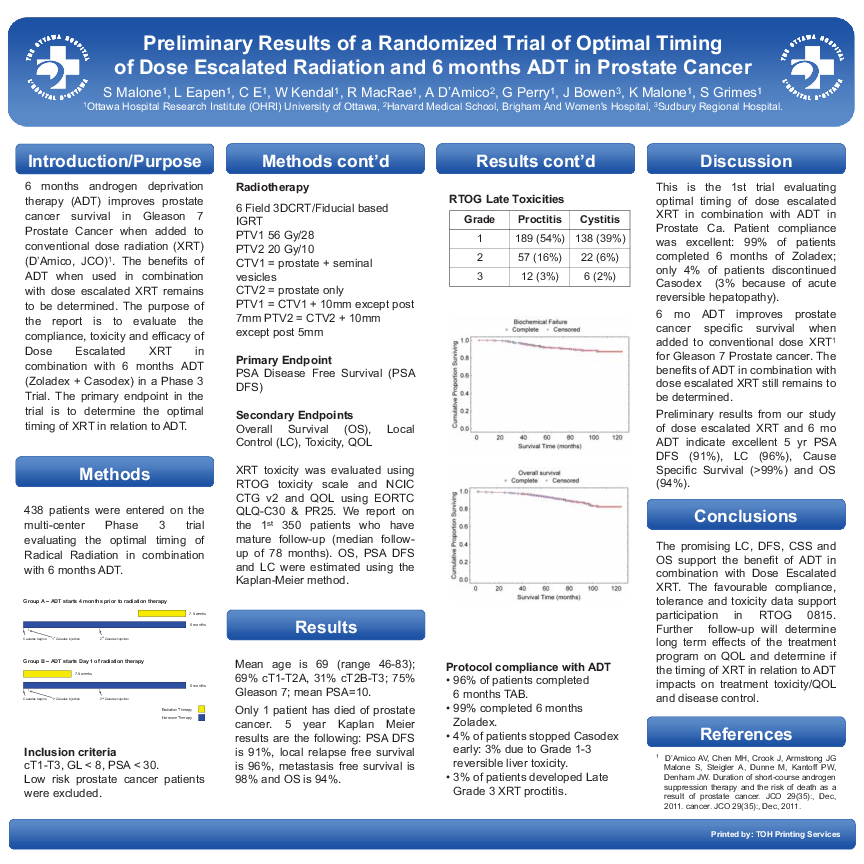
XRT toxicity was evaluated using RTOG toxicity scale and NCIC CTG v2 and QOL using EORTC QLQ-C30 & PR25. We report on the 1st 350 patients who have mature follow-up (median follow- up of 78 months). OS, PSA DFS and LC were estimated using the Kaplan-Meier method.
Results
Mean age is 69 (range 46-83); 69% cT1-T2A, 31% cT2B-T3; 75% Gleason 7; mean PSA=10.
Only 1 patient has died of prostate cancer. 5 year Kaplan Meier results are the following: PSA DFS is 91%, local relapse free survival is 96%, metastasis free survival is 98% and OS is 94%.
RTOG Late Toxicities Grade Proctitis Cystitis
Grade 1, 2 or 3 proctitis: 54%, 16% and 3%. Grade 1, 2 or 3 cystitis 39%, 6% and 2%.
Protocol compliance with ADT
• 96% of patients completed 6 months TAB.
• 99% completed 6 months Zoladex.
• 4% of patients stopped Casodex early: 3% due to Grade 1-3 reversible liver toxicity.
Discussion
This is the 1st trial evaluating optimal timing of dose escalated XRT in combination with ADT in Prostate Ca. Patient compliance was excellent: 99% of patients completed 6 months of Zoladex; only 4% of patients discontinued Casodex (3% because of acute reversible hepatopathy).
6 mo ADT improves prostate cancer specific survival when added to conventional dose XRT1 for Gleason 7 Prostate cancer. The benefits of ADT in combination with dose escalated XRT still remains to be determined.
Preliminary results from our study of dose escalated XRT and 6 mo ADT indicate excellent 5 yr PSA DFS (91%), LC (96%), Cause Specific Survival (>99%) and OS (94%).
Conclusions
The promising LC, DFS, CSS and OS support the benefit of ADT in combination with Dose Escalated XRT. The favourable compliance, tolerance and toxicity data support participation in RTOG 0815. Further follow-up will determine long term effects of the treatment program on QOL and determine if the timing of XRT in relation to ADT impacts on treatment toxicity/QOL and disease control.