Abstract
Introduction:
Bipolar disorders (BPD) are associated with significant risk of suicide. There are several risk factors associated with suicide, however, limited studies have evaluated the relationship between chronic pain disorders (CPD) and suicide among patients admitted for BPD.
Methods:
BPD patients (age ≥18 years) admitted to the hospital were identified from the (NIS) dataset (2016-2018). Based on the secondary diagnosis of CPD, patients were stratified into two groups (1) BPD with CPD (BPD+CPD) and (2) BPD without CPD (BPD-CPD). Groups were matched (1:1) for the type of bipolar disorders and compared for baseline, clinical characteristics, and suicidal ideation/attempt. Logistic regression analysis was performed to assess the predictors associated with suicide.
Results:
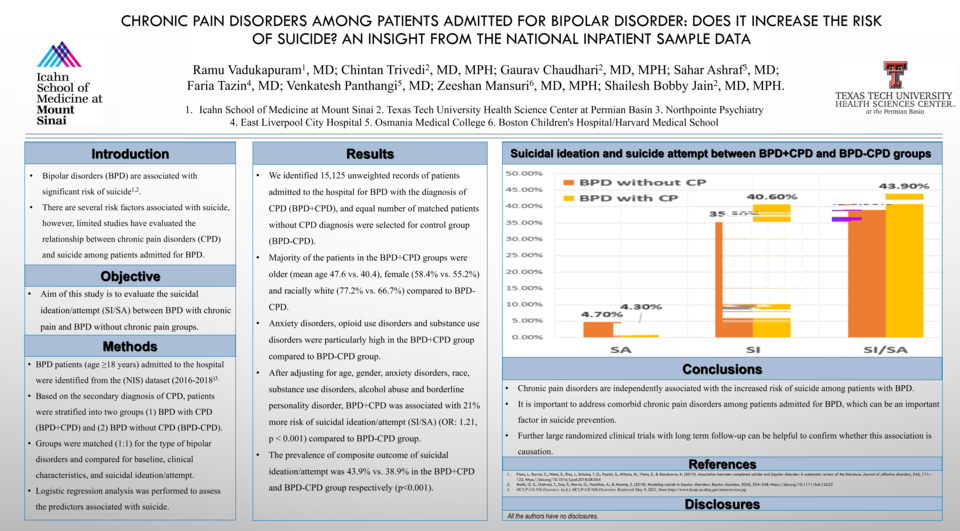
We identified 15,125 unweighted records of patients admitted to the hospital for BPD with the diagnosis of CPD (BPD+CPD), and equal number of matched patients without CPD diagnosis were selected for control group (BPD-CPD). Majority of the patients in the BPD+CPD groups were older (mean age 47.6 vs. 40.4), female (58.4% vs. 55.2%) and racially white (77.2% vs. 66.7%) compared to BPD-CPD. Anxiety disorders, opioid use disorders and substance use disorders were particularly high in the BPD+CPD group compared to BPD-CPD group. After adjusting for age, gender, anxiety disorders, race, substance use disorders, alcohol abuse and borderline personality disorder, BPD+CPD was associated with 21% more risk of suicidal ideation/attempt (SI/SA) (OR: 1.21, p < 0.001) compared to BPD-CPD group. The prevalence of composite outcome of suicidal ideation/attempt was 43.9% vs. 38.9% in the BPD+CPD and BPD-CPD group respectively (p<0.001).
Conclusion:
Chronic pain disorders are independently associated with the increased risk of suicide among patients with BPD. It is important to address co-morbid chronic pain disorders among patients admitted for BPD, which can be an important factor in suicide prevention. Further large randomized clinical trials with long term follow-up can be helpful to confirm whether this association is causation.