Abstract
Introduction
Neurological complications in COVID-19 infected patients have not been widely reported. Since elderly patients with chronic medical conditions are at an increased risk of altered mental status in the setting of acute infections, patients with COVID-19 infection can also present with acute encephalopathy and changes in their level of consciousness. Here we report a patient that presented with encephalopathy and was found to be infected with COVID-19.
Case Description:
A 74-year-old male with a past medical history significant for atrial fibrillation, previous cardioembolic stroke, Parkinson Disease, chronic obstructive pulmonary disease presented to the emergency department with a chief complaint of fever, cough and altered mental status.
Patient recently traveled to he Netherlands and had presented to our facility only seven days after arriving to the United States.
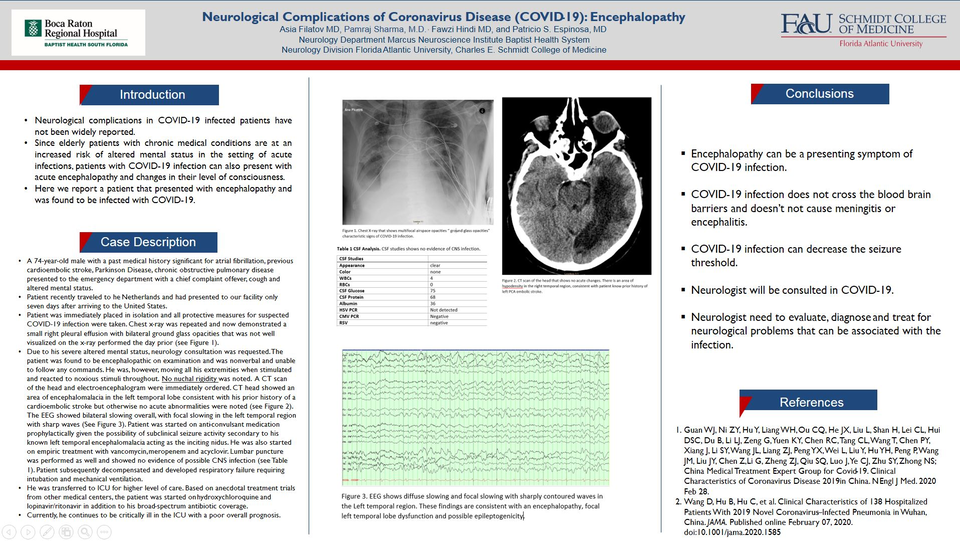
Patient was immediately placed in isolation and all protective measures for suspected COVID-19 infection were taken. Chest x-ray was repeated and now demonstrated a small right pleural effusion with bilateral ground glass opacities that was not well visualized on the x-ray performed the day prior (see Figure 1).
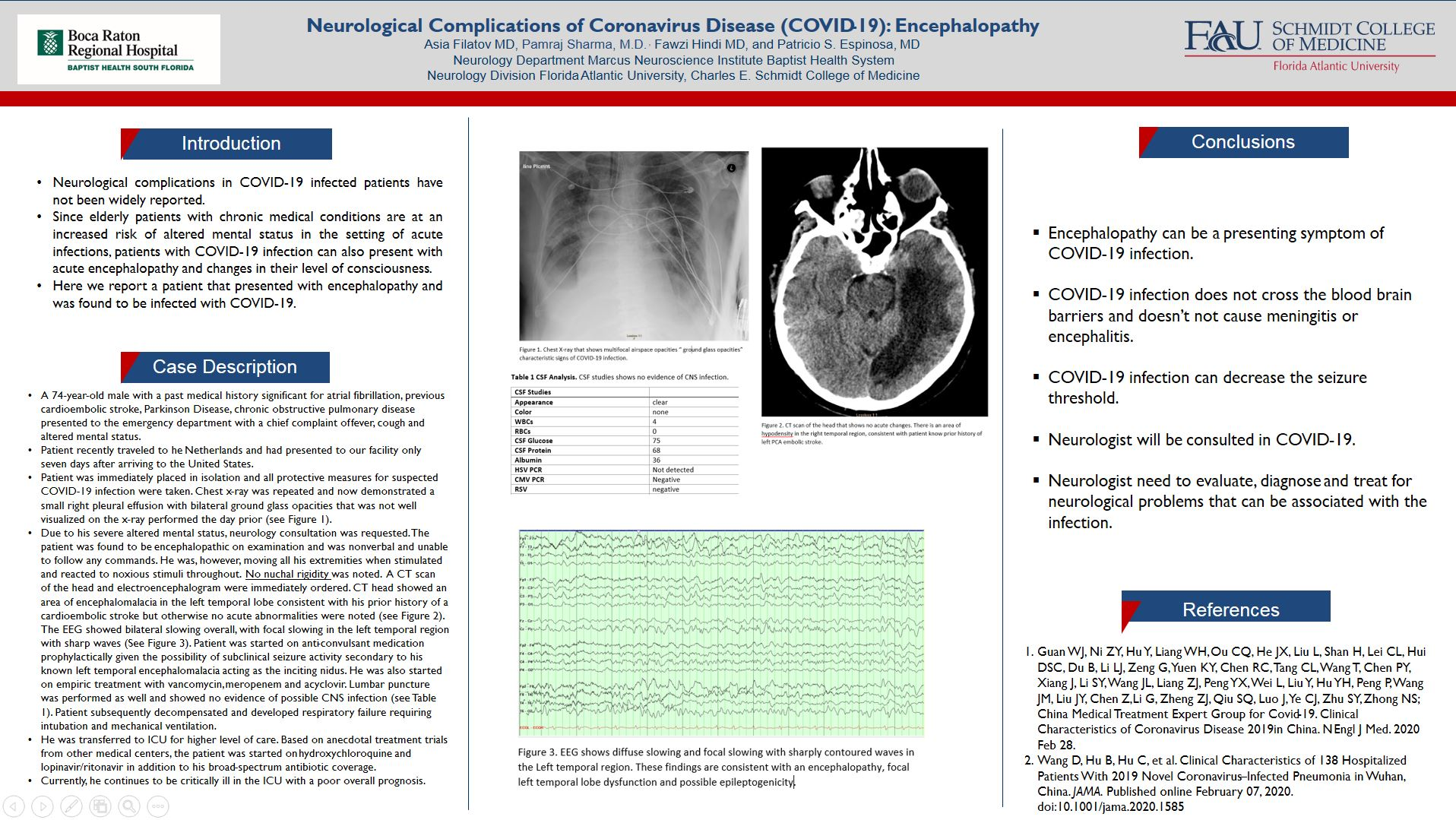
Due to his severe altered mental status, neurology consultation was requested. The patient was found to be encephalopathic on examination and was nonverbal and unable to follow any commands. He was, however, moving all his extremities when stimulated and reacted to noxious stimuli throughout. No nuchal rigidity was noted. CT head showed an area of encephalomalacia in the left temporal lobe consistent with his prior history of a cardioembolic stroke but otherwise no acute abnormalities were noted (see Figure 2). The EEG showed bilateral slowing overall, with focal slowing in the left temporal region with sharp waves (See Figure 3). Patient was started on anti-convulsant medication prophylactically given the possibility of subclinical seizure activity secondary to his known left temporal encephalomalacia acting as the inciting nidus. He was also started on empiric treatment with vancomycin, meropenem and acyclovir. Lumbar puncture was performed as well and showed no evidence of possible CNS infection (see Table 1). Patient subsequently decompensated and developed respiratory failure requiring intubation and mechanical ventilation.
He was transferred to ICU for higher level of care. Based on anecdotal treatment trials from other medical centers, the patient was started on hydroxychloroquine and lopinavir/ritonavir in addition to his broad-spectrum antibiotic coverage.
Currently, he continues to be critically ill in the ICU with a poor overall prognosis.
Conclusions:
Encephalopathy can be a presenting symptom of COVID-19 infection.
COVID-19 infection does not cross the blood brain barriers and doesn’t not cause meningitis or encephalitis.
COVID-19 infection can decrease the seizure threshold.
Neurologist will be consulted in COVID-19.
Neurologist need to evaluate, diagnose and treat for neurological problems that can be associated with the infection.
References:
1.Guan WJ, et al; China Medical Treatment Expert Group for Covid-19. Clinical Characteristics of Coronavirus Disease 2019in China. N Engl J Med. 2020 Feb 28.
2.Wang D, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China. JAMA. Published online February 07, 2020.