Abstract
Background
Several neoadjuvant multimodality strategies have been developed to improve low resectability rates in pancreatic ductal adenocarcinoma (PDAC). Neoadjuvant SBRT accurately delivers high doses of conformal radiation in theoretically ablative doses, appearing to offer acceptable local control and survival outcomes. Yet it is unknown if neoadjuvant SBRT improves clinical outcomes due to differences in radiographic, clinical and pathological response. This study aimed to synthesize published evidence on neoadjuvant SBRT for PDAC.
Materials and Methods
The Cochrane Library, Medline, PubMed and EMBASE were systematically searched to identify full-text publications with original data on the neoadjuvant use of SBRT in PDAC. R0 resection rate was the primary endpoint. Secondary endpoints included dose and fractionation regimens, grade 3+ toxicities, resectability rates, pathological response rates and survival outcomes.
Results
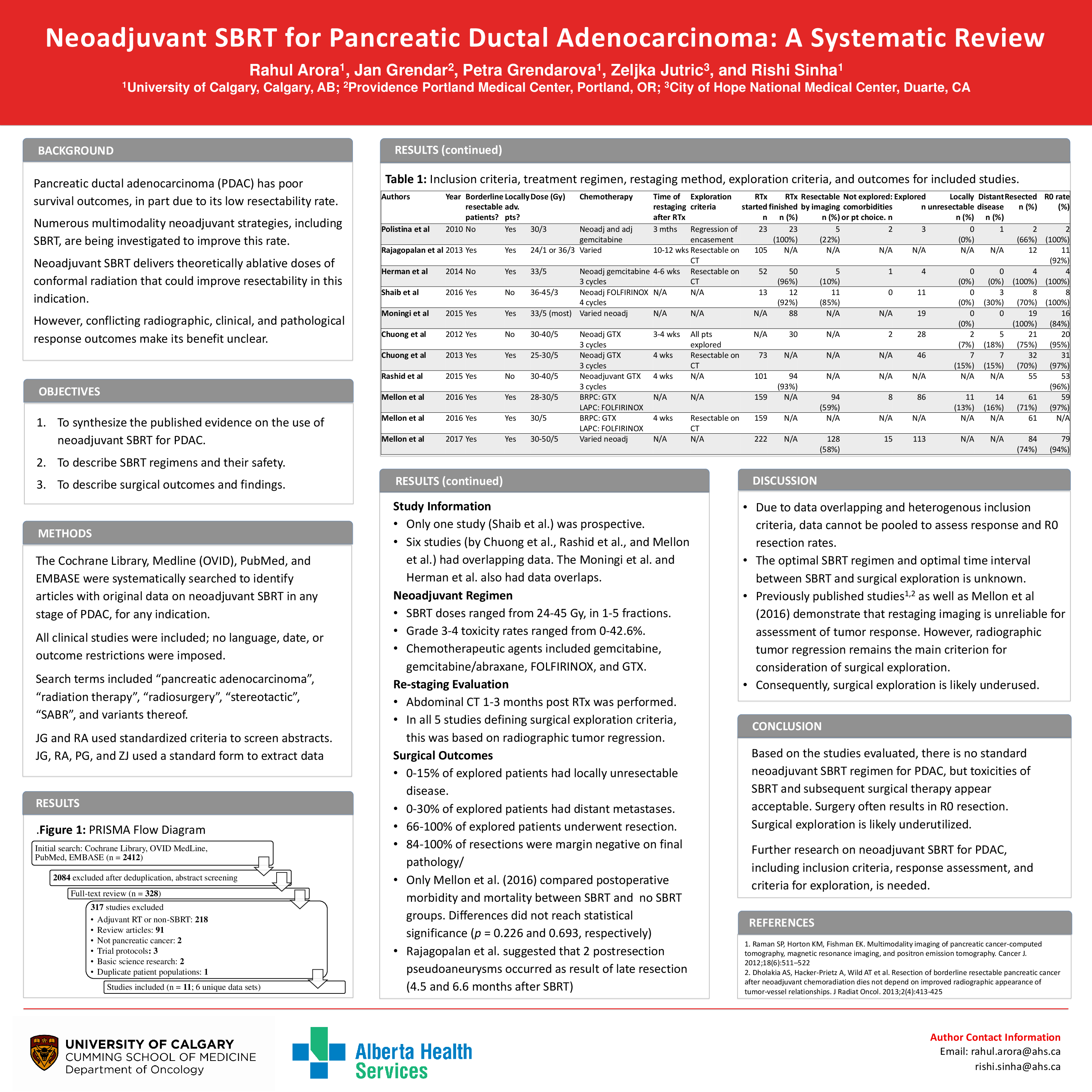
Of 1448 screened abstracts, we included 327 publications for full-text review. Six studies met inclusion criteria and were included in the present analysis – 4 retrospective single institution studies, 1 prospective phase 1 trial and 1 prospective phase 2 trial. 7 additional publications described subsets of already included patients and were not included in this review. A total of 345 patients (0 upfront resectable, 144 borderline resectable with varying definitions and 201 locally advanced) underwent neoadjuvant SBRT with 25-50 Gy in 1-5 fractions. Acute grade 3+ toxicity occurred in 0-28.4% and late grade 3+ toxicities in 0-16.7% of patients. 96% of patients received neoadjuvant chemotherapy prior to SBRT (75% gemcitabine based, 25% FOLFIRINOX). Surgical exploration was performed 0.1-10.5 months after SBRT in 8-100% of patients if no progression or radiographic response was seen. Of those, 66-100% of patients underwent resection, with 84-100% R0 resections. No formal intraoperative tissue assessment or postoperative morbidity or mortality was described; studies only mention expected perioperative outcomes. One study suggested an association between complications and a prolonged SBRT-resection interval. 5 studies described pathological response rates. Complete pathological response occurred in 12.2% and no or poor response in 11.4% of specimens. Node negative disease was found in 63% of specimens. Overall survival was 11-47.2 months and disease-free survival 5.7-27.4 months.
Conclusions
There is no standard dosing or timing of neoadjuvant SBRT for PDAC. Subsequent surgical therapy appears safe, frequently resulting in R0 resection with acceptable toxicity. Based on evaluated literature, surgical exploration is likely underutilized. Development of multi-institutional, multidisciplinary prospective registries has the potential to identify optimal SBRT protocols and maximize treatment options for PDAC patients.