Abstract
Purpose
Spinal disease (SD) in Myeloma (MM) presents with lytic lesions, compression fractures or spinal cord compression (SCC). We set out to assess the incidence of SD in newly diagnosed MM patients and to document its survival impact with and without spinal radiotherapy (RT).
Methods
Using the provincial cancer registry, all MM patients diagnosed between 2010 and 2015 were identified and reviewed. SD was defined as osteolytic vertebral lesions, compression fractures or SCC documented within 3 months of diagnosis on X-ray, CT scan or MRI. Incidence of SD and survival of patients with and without SD was determined. For patients with SD, we compared survival of those treated with or without spinal RT within 3 months of diagnosis. Effect of RT dose/fractionation, number of chemotherapy cycles and treatment with autologous stem cell transplant (ASCT) was also described.
Results
Three hundred and six patients were identified. Mean age was 69 years and 173 were male (56.5%). Two hundred and ninety patients (95%) had plain x-ray, 190 (62%) had CT spine and 109 (36%) had MRI spine. One hundred and fifty-five (50.7%) had documented SD, 120 (39.2%) had compression fractures and 24 (7.8%) had SCC. Most patients received chemotherapy (273 or 89.2%) and 69 (22.5%) received ASCT.
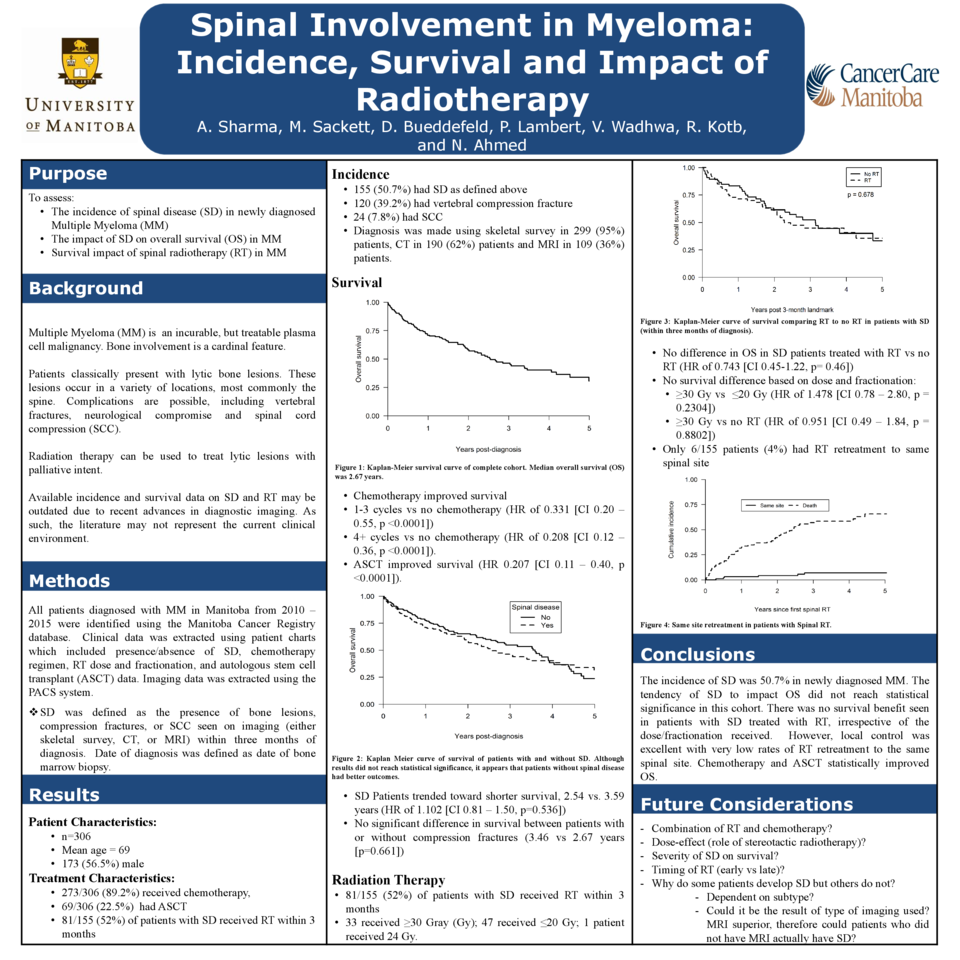
Overall survival (OS) was 2.67 years for the entire cohort. Patients with SD showed tendency toward shorter survival (2.54 vs 3.59 years), but this did not reach statistical significance (HR of 1.102 [CI 0.81 – 1.50, p=0.536]). There was also no statistically significant survival difference between patients with or without compression fractures (2.67 vs 3.46 years [p=0.661]).
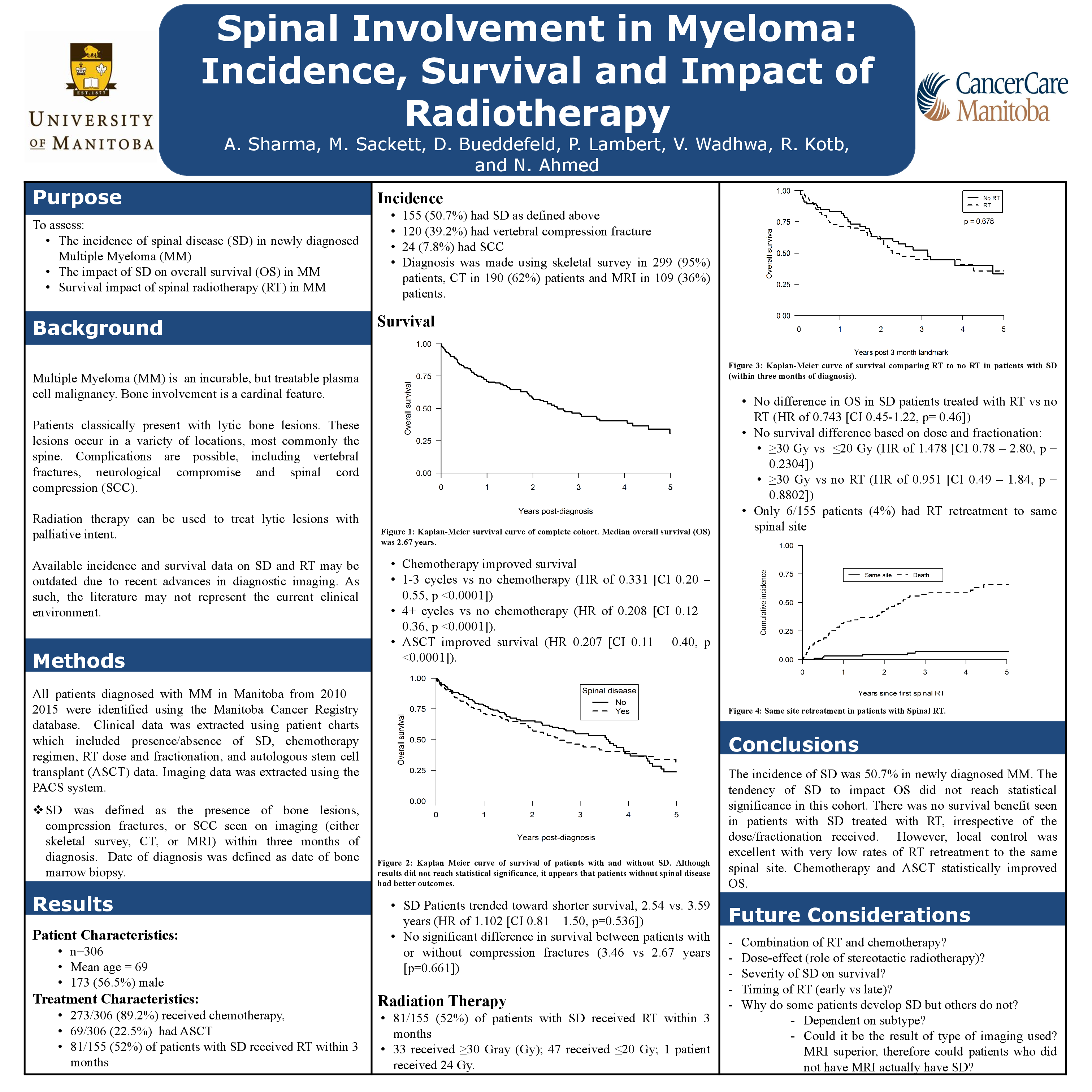
Only 81/155 (52%) patients with SD received spinal RT within 3 months of diagnosis. Of these, 33 received ≥30 Gray (Gy) and 47 received ≤20 Gy. One patient received 24 Gy.
There was no difference in OS of patients with spinal disease, with or without spinal RT (HR of 0.743 [CI 0.45-1.22, p= 0.46]). There was no survival difference based on total dose/fractionation: ≥30 Gy vs ≤20 Gy (HR of 1.478 [CI 0.78 – 2.80, p = 0.2304]) and ≥30 Gy vs no RT (HR of 0.951 [CI 0.49 – 1.84, p = 0.8802]).
Patients who received chemotherapy had improved survival: 1-3 cycles vs no chemotherapy (HR of 0.331 [CI 0.20 – 0.55, p <0.0001]) and 4+ cycles vs no chemotherapy (HR of 0.208 [CI 0.12 – 0.36, p <0.0001]). Also, patients who received ASCT had improved survival (HR 0.207 [CI 0.11 – 0.40, p <0.0001]).
Conclusion
The incidence of SD was 50.7% in newly diagnosed MM. The tendency of SD to impact OS did not reach statistical significance in this cohort. There was no survival benefit seen in patients with SD treated with RT, irrespective of the dose/fractionation received. Chemotherapy and ASCT statistically improved OS.