Abstract
Purpose
Radiation is one of the modalities used to treat non-melanoma skin cancers. For facial lesions; ortho-voltage radiotherapy (RT) can require the creation of lead shielding to protect vulnerable organs at risk (OAR). Creating a lead shield is often difficult due to the complex contours of the face. The traditional method involves creating a plaster mould of a patient’s face to use as a template for creating a shield. This requires another patient visit, and for patients who are claustrophobic or medically unable to lie flat, this strategy is not ideal. We address this by utilizing optical scanner and 3D printer technology to create lead shields and report the first case series in the English literature here.
Materials
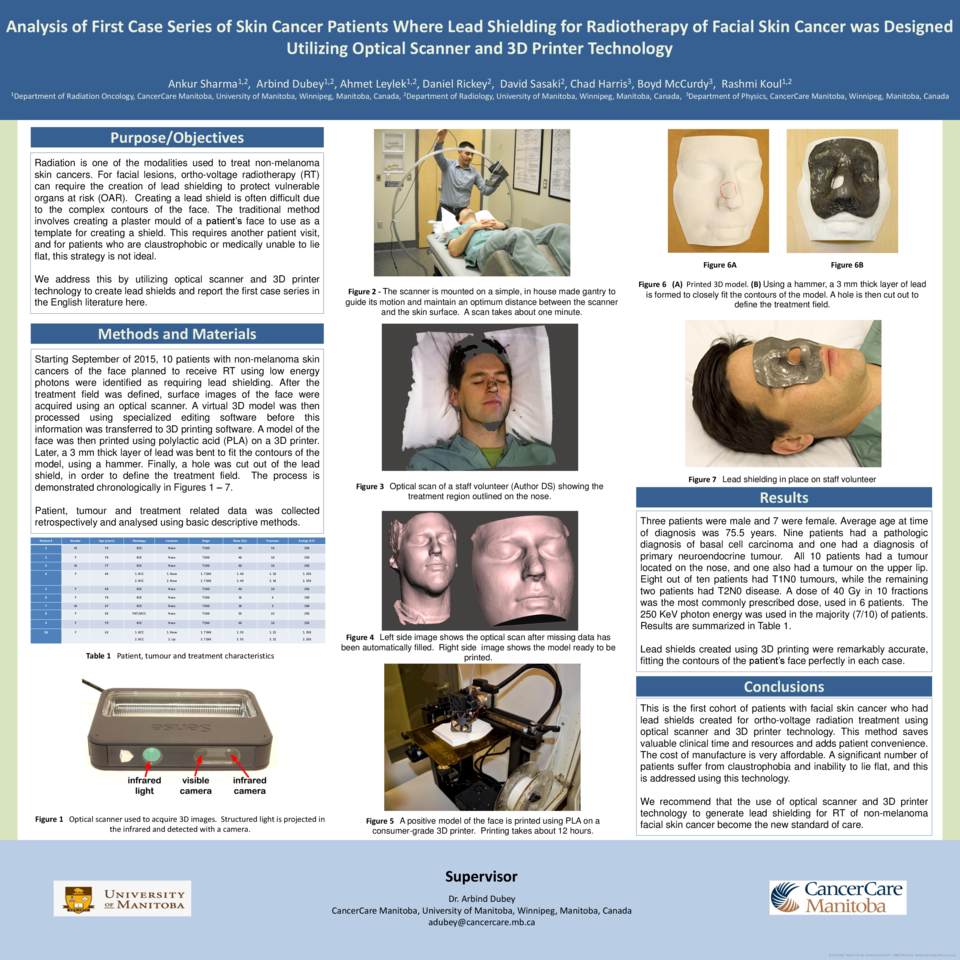
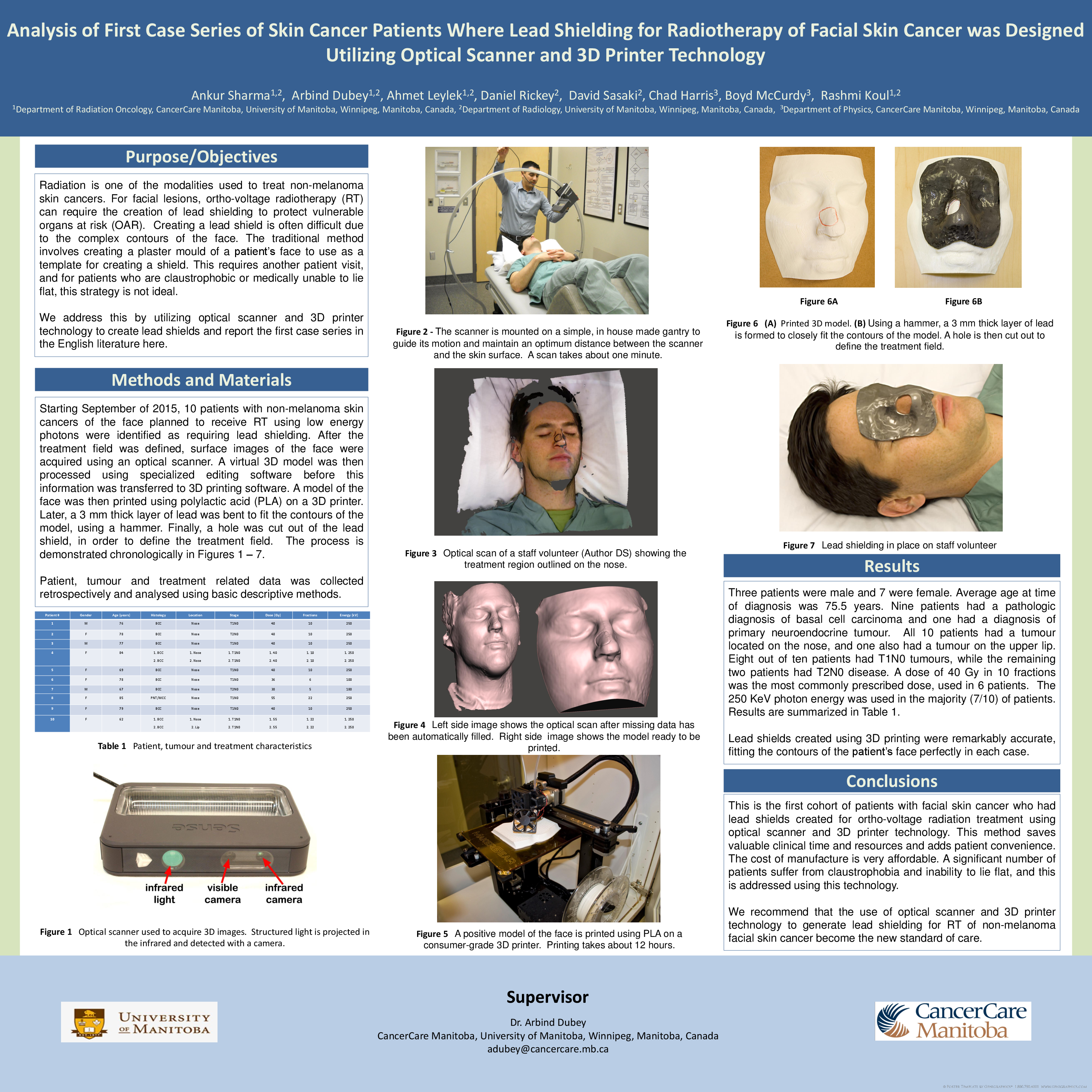
Starting September of 2015, 10 patients with non-melanoma skin cancers of the face planned to receive RT using low energy photons were identified as requiring lead shielding. After the treatment field was defined, surface images of the face were acquired using an optical scanner. A virtual 3D model was then processed using specialized editing software before this information was transferred to 3D printing software. A model of the face was then printed using polylactic acid on a 3D printer. Later, a 3 mm thick layer of lead was bent to fit the contours of the model, using a hammer. Finally, a hole was cut out of the lead shield, in order to define the treatment field.
Patient, tumour and treatment related data was collected retrospectively and analyzed using basic descriptive methods.
Results
Three patients were male and 7 were female. Average age at time of diagnosis was 75.5. 9 patients had a pathologic diagnosis of basal cell carcinoma and one had a diagnosis of primary neuroendocrine tumour. All 10 patients had tumour on the nose, and one also had a tumour on the upper lip. 8/10 patients had T1N0 tumour stage, while in the remaining two it was T2N0. 40 Gy in 10 fractions was the most commonly prescribed dose in 6 patients. 250 KeV was the chosen photon energy in the majority (7/10) of patients.
Lead shields created using 3D printing were remarkably accurate, fitting the contours of the patient’s face perfectly in each case.
Conclusion
This is the first cohort of patients with facial skin cancer who had lead shields created for ortho-voltage radiation treatment using optical scanner and 3D printer technology. This method saves valuable clinical time and resources and adds patient convenience. The cost of manufacture is also very affordable. A significant number of patients suffer from claustrophobia and inability to lie flat, and this is addressed using this technology. We recommend that the use of optical scanner and 3D printer technology to generate lead shielding in RT of non-melanoma facial skin cancer become the new standard of care.