Abstract
Background:
Radiotherapy (RT) practice variability in the palliative setting is well-documented. Clinical practice guidelines inform standardized, evidence-based, beneficial practice, while simultaneously discouraging unnecessary or potentially harmful practices. The process of creating provincial palliative RT clinical practice guidelines is associated with multiple challenges. We describe the unique approach required in aligning multidisciplinary goals as compared to traditional tumour site-specific guidelines.
Methods:
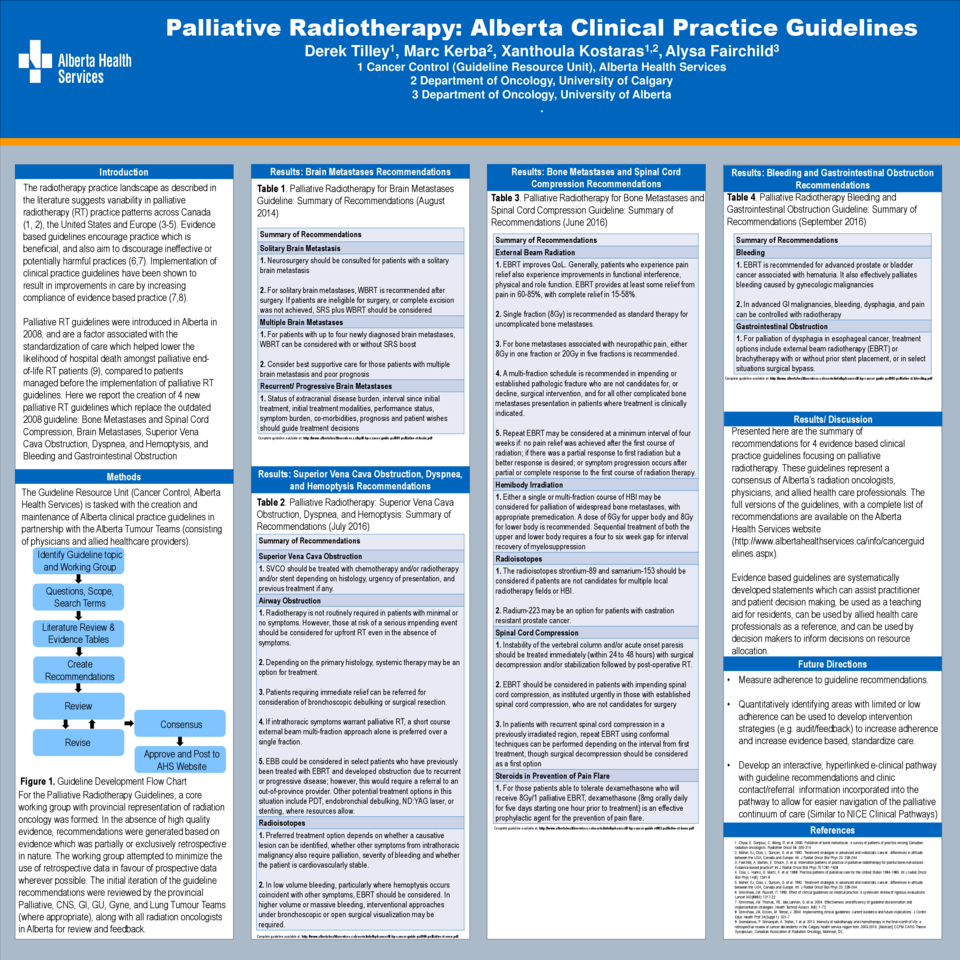
Radiation oncologists from the provincial Palliative Care Tumour Team, along with guideline specialists from the Guideline Resource Unit, formed the primary guideline working group tasked with updating the Palliative RT guidelines. Tumour site specific representatives (ex. Central Nervous System Tumour Team) were incorporated as needed, as well as experts in supportive care, on a guideline by guideline basis. For each guideline, a systematic literature review was conducted to identify relevant evidence. Recommendations were initially developed within the primary working group, then revised in collaboration with experts from other disciplines. Once working group consensus was reached, guideline recommendations were circulated to all radiation oncologists and Palliative Tumour Team members for input. After several rounds of feedback and modifications, provincial consensus was reached.
Results:
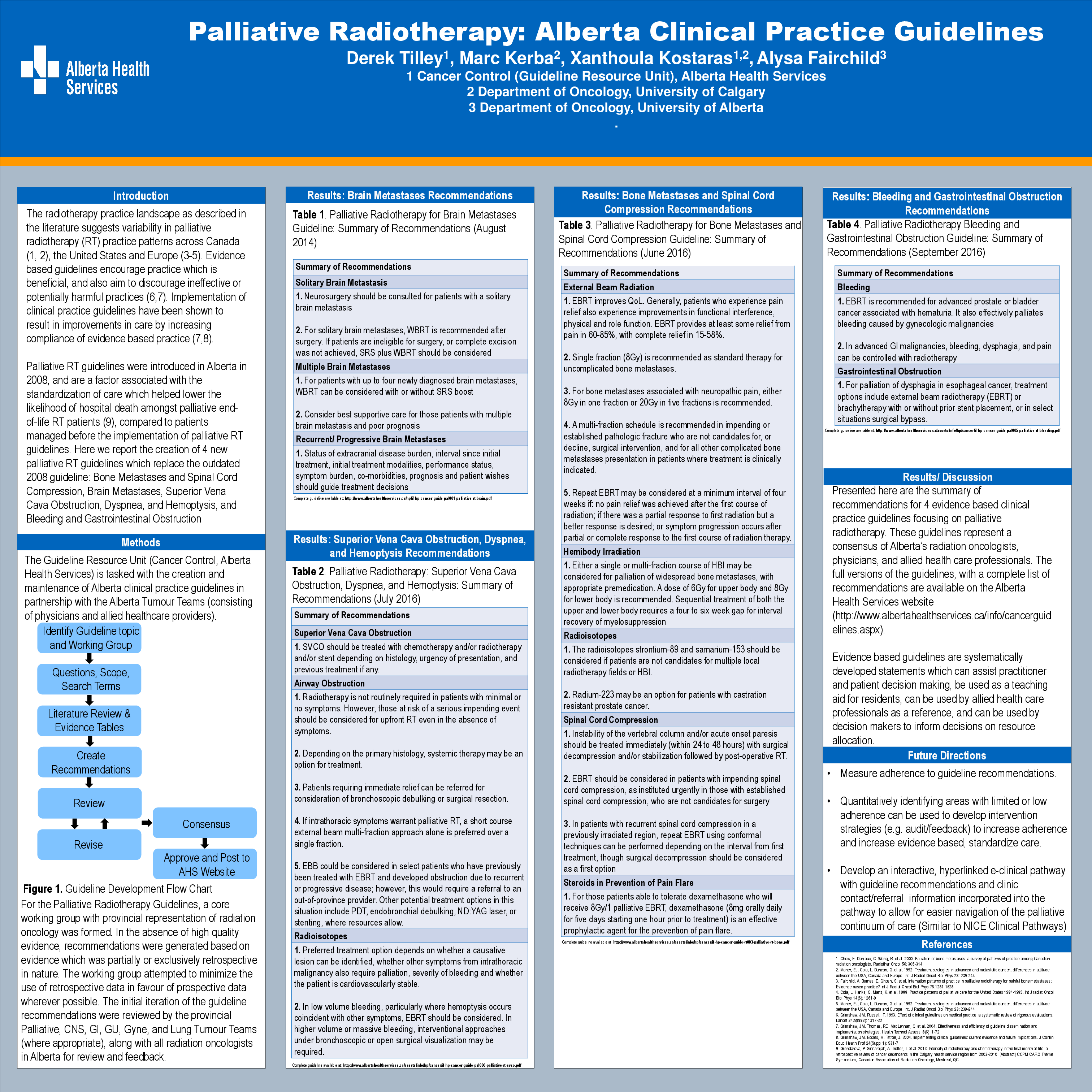
Initially, one RT guideline had been created for all provincial palliative RT recommendations. These guidelines have since been split into smaller, more functional palliative RT guidelines: (1) Brain Metastases; (2) Bone Metastases and Spinal Cord Compression; (3) Bleeding and Gastrointestinal Obstruction; and (4) Superior Vena Cava Obstruction, Dyspnea, and Hemoptysis. The majority of recommendations were either modified or new due to advancements in research or changes in consensus based approaches. In total, 70 recommendations were approved. Recommendations were supported by a range of evidence from high (level one evidence) to low quality (consensus opinion).
Conclusion:
By combining the newly updated palliative RT guidelines with an educational intervention, variations in practice MAY be mitigated. Using our model, similar efforts can be undertaken in other jurisdictions.