Abstract
Purpose: The standard treatment for men with newly diagnosed metastatic prostate cancer (mPCa) is androgen deprivation therapy (ADT). Local radiotherapy (RT) to the prostate has traditionally been reserved for men who require symptomatic relief in patients with metastatic disease. However, local RT may have other benefits in addition to symptomatic relief. This study investigates the impact of local RT on overall survival (OS) in men with newly diagnosed mPCa.
Materials and Methods: This is a retrospective, population-based study of patients age >= 18 years diagnosed with metastatic (M1) prostate cancer in Manitoba between 2004-2013. Patients with neuroendocrine or small cell histology were excluded. Data was collected from Cancer Registry and electronic charts including age, T/N/M stage, PSA, Charlson comorbidity score, RT, surgery, systemic therapy, Gleason score, and ECOG performance status. Cox regression was used to predict OS. Likelihood ratio testing was used to identify factors associated with OS. A p value <0.05 was considered significant.
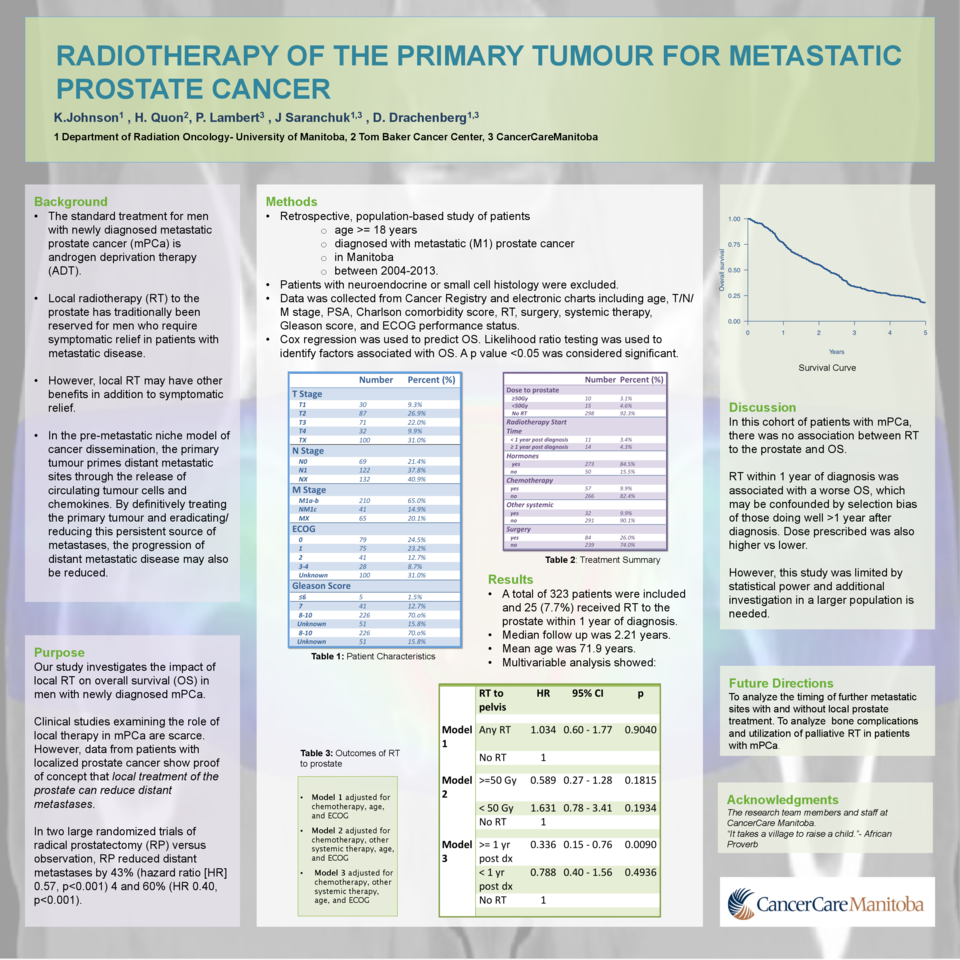
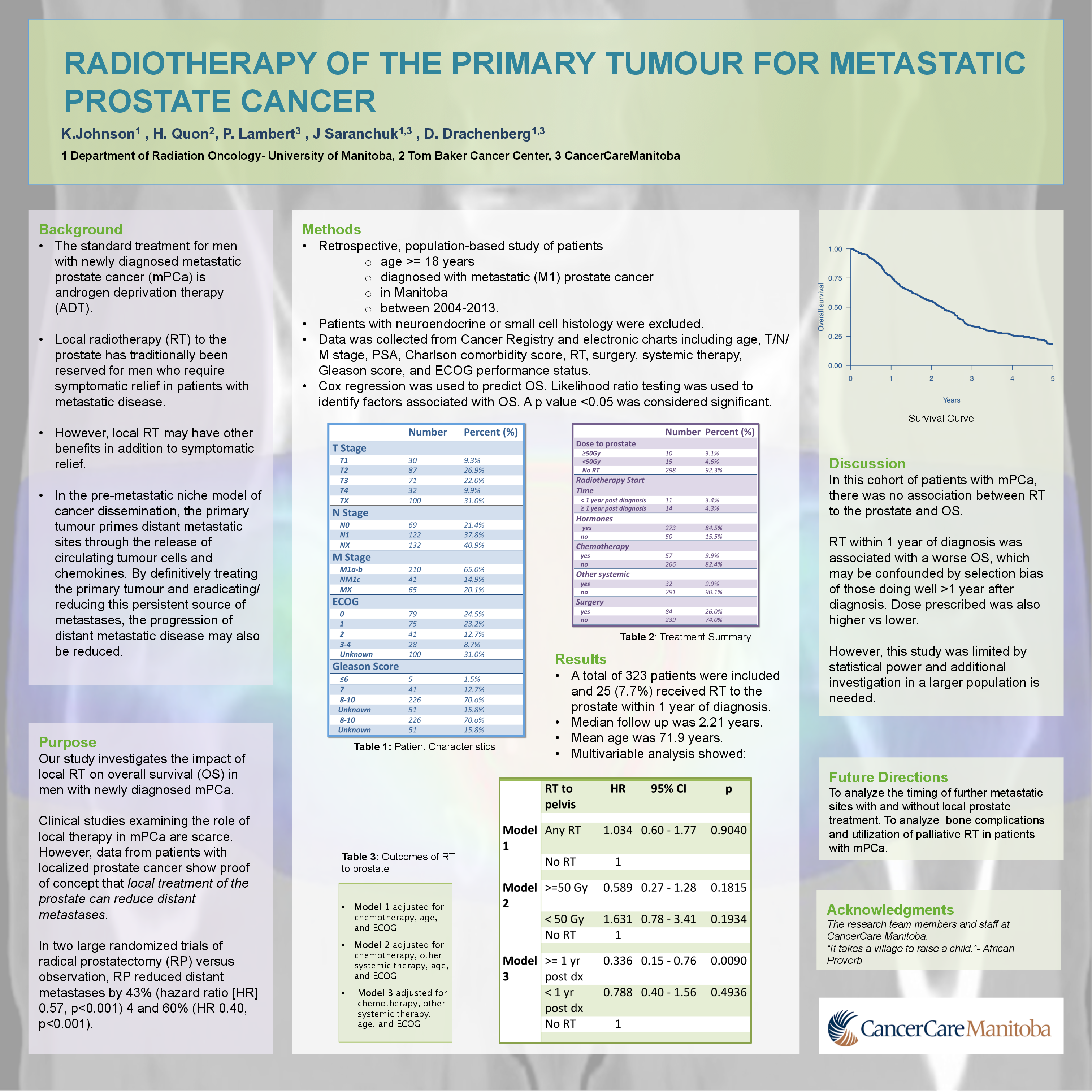
Results: A total of 323 patients were included and 25 (7.7%) received RT to the prostate within 1 year of diagnosis. The median follow up was 2.21 years. The mean age was 71.9 years. Clinical T stage included T1 (9.3%), T2 (26.6%), T3 (21.7%) and T4 (10.5%) and TX (31.9%), N stage ranged from N0 (21.4%), N1 (37.5%), NX (41.2%). M stages consisted of M1a/M1b (63.5%), M1c (14.2%) or MX (22.3%). Of the 25 patients who received prostate RT, 15 received high dose (≥ 50 Gy) and 10 low dose (<50 Gy). Multivariable analysis showed a hazard ratio (HR) for death of 1.09 (95% CI 0.64-1.85, p=0.75) for patients receiving prostate RT (any dose) compared to those without prostate RT. The HR for high dose RT was 0.59 (95% CI 0.27-1.28, p=0.2) and 1.63 (95% CI 0.78-3.41, p=0.2) for low dose RT. Furthermore, the HR was 0.336 (95% CI 0.15-0.76, p=0.01) for those patients who received RT later than one year after time of diagnosis.
Conclusions: In this cohort of patients with newly diagnosed mPCa, there was no association between RT to the prostate and OS. However, a trend towards increased OS in this patients receiving high dose local RT and those well enough to receive RT greater than one year out of diagnosis was observed. This study was limited by statistical power and additional investigation in a larger population is needed.