Abstract
Objective: Patient and family-centered care (PFCC) represents an evolution from traditional models of provider-focused and patient-focused care that places a strong emphasis on optimal patient communication, patient autonomy, and shared decision-making within care teams. A shift towards PFCC requires participation across all provider groups. Despite the importance of physician buy-in, research examining physicians’ perspectives on PFCC is lacking. We sought to explore oncologists’ familiarity with the principles of PFCC, perceived barriers to implementing principles of PFCC, and examples of physician behaviours consistent with PFCC.
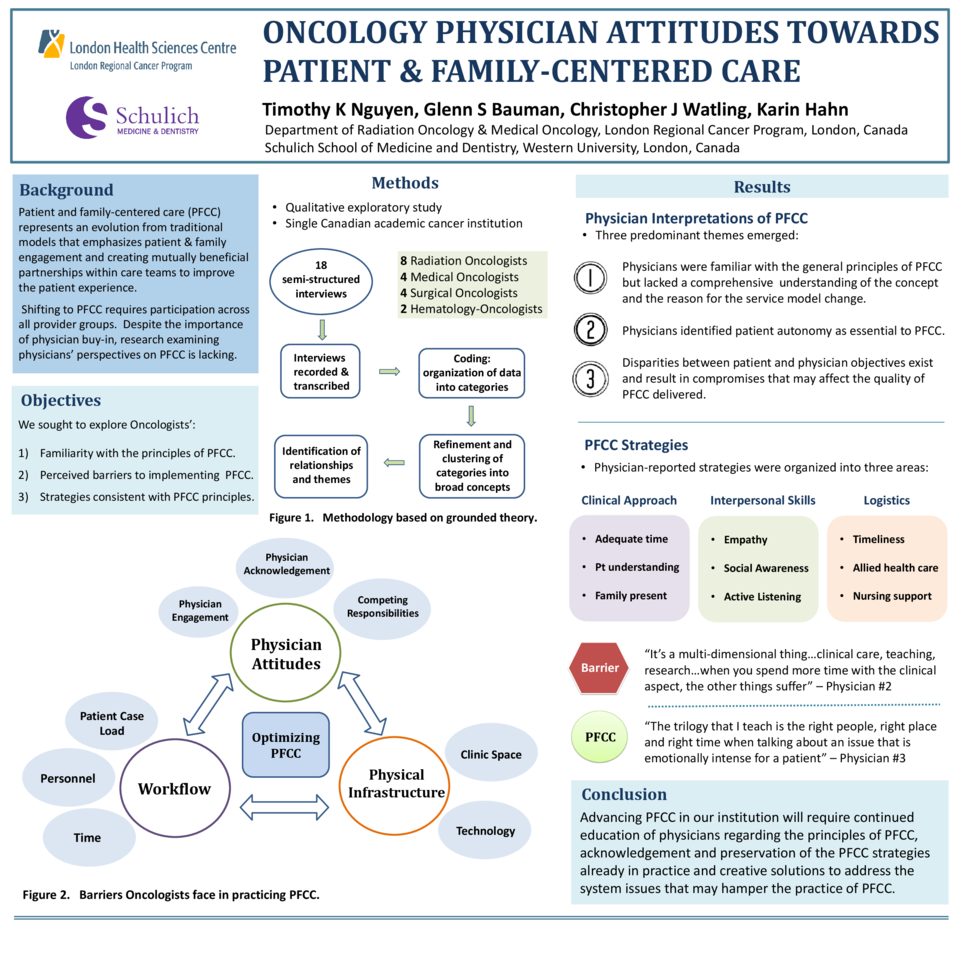
Methods: In this qualitative exploratory study, we conducted semi-structured interviews with 18 oncologists (8 radiation, 4 medical, 4 surgical, 2 hematologist-oncologists) at a single Canadian academic cancer institution. Interview data were analyzed using coding principles drawn from grounded theory. Constant comparisons were used to identify recurring themes.
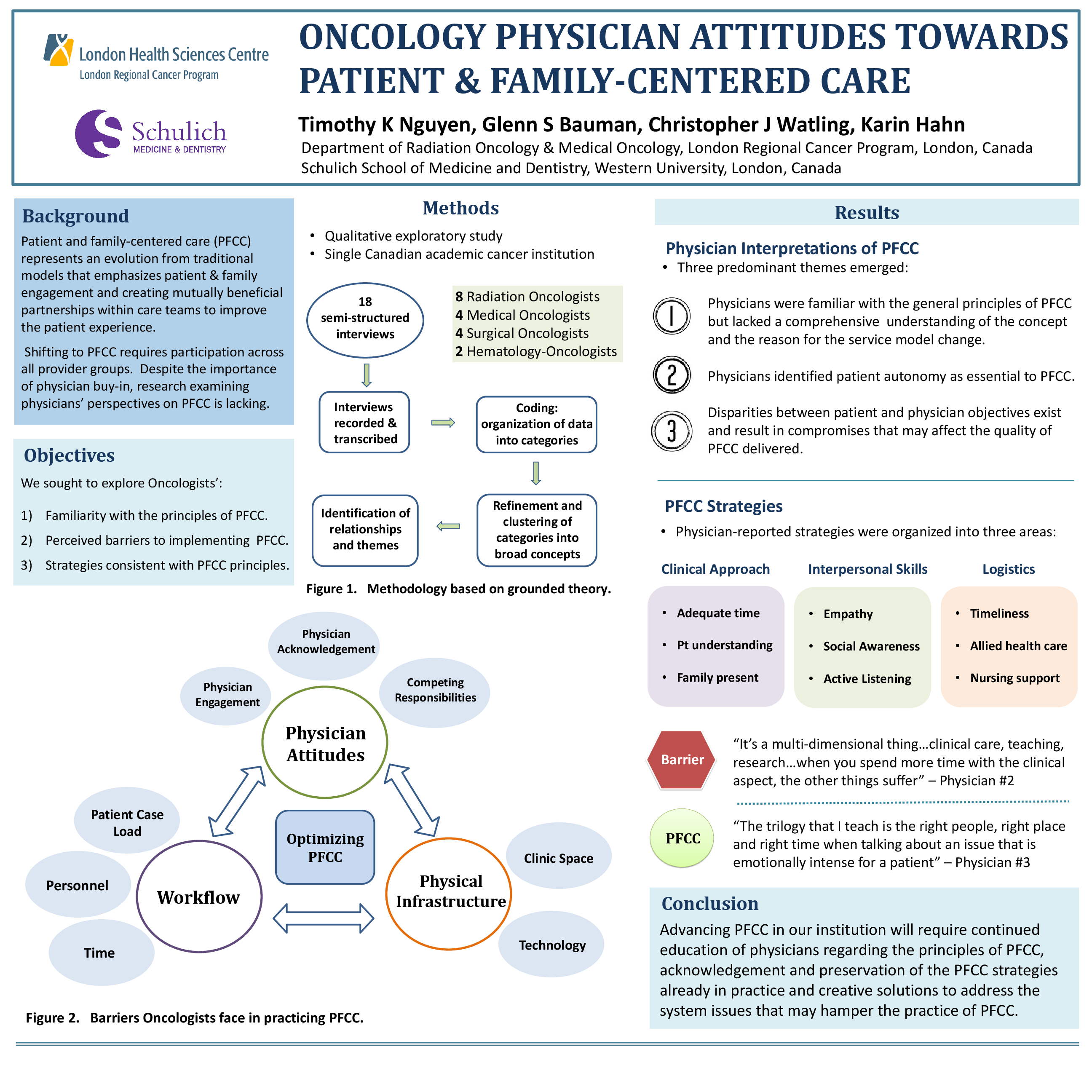
Results: We identified 3 dominant themes related to physicians’ interpretations of PFCC: 1) Physicians expressed a limited understanding of the formal principles of PFCC, 2) Physicians identified patient autonomy as essential to PFCC and 3) Disparities between patient and physician objectives exist and result in compromises that may affect the quality of PFCC delivered. Time was both a facilitator and a barrier. While oncologists perceived that spending more time with patients improved PFCC, they also recognized that time was limited: spending more time engaging in PFCC would leave less time to devote to other necessary activities. Participants also identified a number of ‘system’ barriers to PFCC, including limited staff and clinical space, excessive case load, a lack of physician support and input into operational decisions, and funding constraints. Many felt that PFCC was challenged by inefficiencies in the system of care delivery, and that progress might lie in reorganization that more clearly matched health care staff’s roles and responsibilities to their credentials and skills. Self-identified behaviours enabling PFCC generally involved strategies to ensure patient needs were met despite time constraints and remaining attentive to the clinical environment in order to provide care appropriate to individual patient experiences.
Conclusions: Based on our interviews, advancing PFCC in our institution will require continued education of physicians regarding the principles of PFCC, acknowledgement and preservation of the PFCC behaviors already in practice and creative solutions to address the system issues that may hamper their abilities to enact PFCC.