Abstract
Purpose: Over the course of radiation therapy treatments for head and neck (H&N) cancers, many patients’ contours change shape due to weight loss. This affects the fit of the shell, and the shape of the planned dosimetric volumes. There are a variety of methods used to measure the change in a patients’ external contour over the course of their treatment. Investigation is needed to determine the effectiveness of these methods.
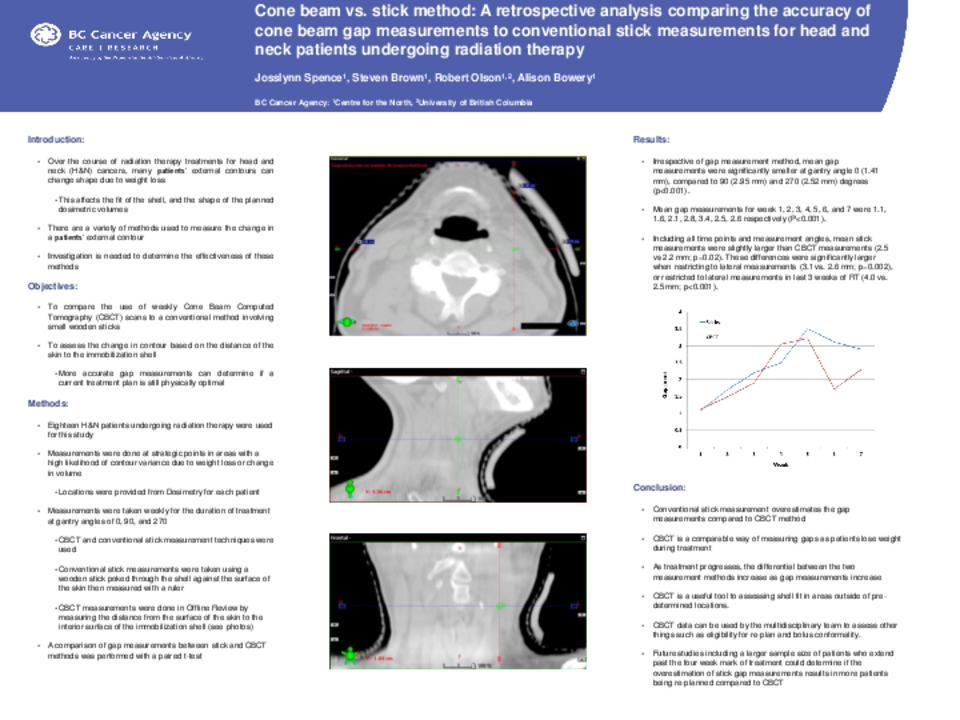
Objective: To complete a retrospective analysis that compares the weekly use of Cone Beam Computed Tomography (CBCT) to a conventional method involving small wooden sticks. These methods assess the change in contour based on the distance of the skin to the immobilization shell.
Methods: Measurements from eighteen H&N patients undergoing radiation therapy were used for this study. Strategic measurement points in areas with a high likelihood of contour variance due to weight loss or change in volume were provided from Dosimetry for each patient. Measurements were taken at gantry angles of 0, 90, and 270 once per week using both CBCT and conventional stick measurement techniques for the duration of treatment. A comparison of gap measurements between stick and CBCT methods was performed with a paired t-test.
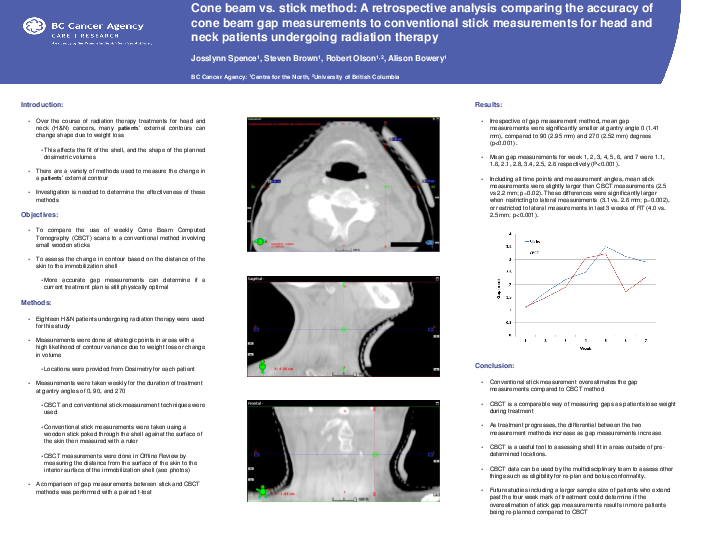
Results: Irrespective of gap measurement method, mean gap measurements were significantly smaller at 0 (1.41 mm), compared to 90 (2.95 mm) and 270 (2.52 mm) degrees (p<0.001). Mean gap measurements for week 1, 2, 3, 4, 5, 6, and 7 were 1.5, 2.0, 2.3, 3.3, 4.0, 3.1, and 3.0, respectively (P<0.001). Including all time points and measurement angles, mean stick measurements were slightly larger than CBCT (2.5 vs 2.2 mm; p=0.02), though these differences were significantly larger when restricting to lateral measurements (3.1 vs. 2.6 mm; p=0.002), or restricted to lateral measurements in last 3 weeks of RT (4.0 vs. 2.5 mm; p<0.001).
Conclusion:
Overall, conventional stick method overestimates the gap measurements compared to CBCT method. As treatment progresses, the gap measurements increase as well as the differential between the two methods. Future studies including a larger sample size of patients that extend past the four week mark of treatment could determine if the overestimation of stick gap measurements results in more patients being re-planned compared to CBCT.