Abstract
Context
The simulation-enhanced Perioperative Nurse Residency Program at Yale New Haven Hospital was developed to address a high vacancy rate due to aging workforce and applicant pool with limited operating room experience; and a need to decrease cost of orientation. The goals of the program were to decrease length of orientation, improve retention rate and train perioperative nurses who are competent and confident. The structure of the program allows educators to train newly hired nurses on basic skill sets that transcend adult and pediatric patient populations but also explore the nuances of pediatric, adult, and each surgical subspecialty.
Description
An inter-professional design team comprised of simulation experts, nursing leadership, and key stakeholders from perioperative nursing used organizational change models to design the program. Over several sessions, the team brainstormed ideal structure and support; and defined essential content, organization of content, learning modalities, and methods to assess learning. Following these sessions, a smaller working group was formed to continue to build.
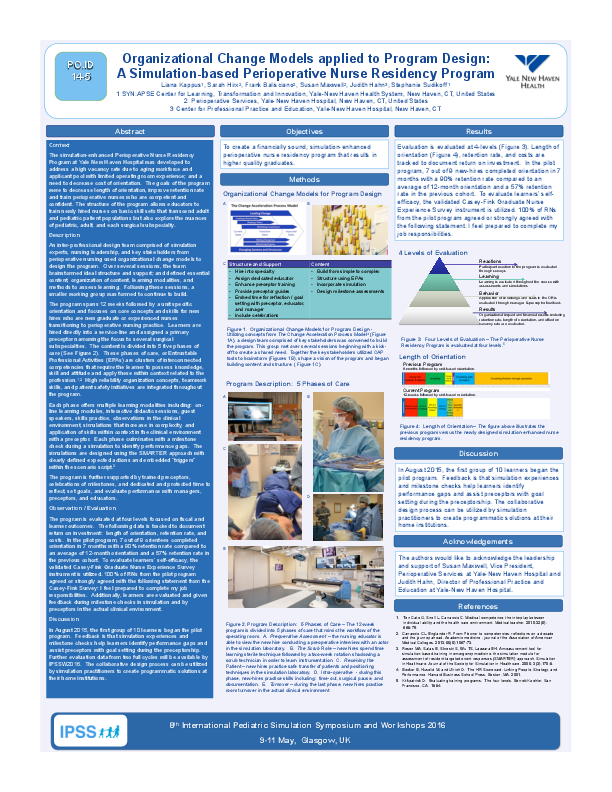
The program spans 12 weeks followed by a unit specific orientation and focuses on core concepts and skills for new hires who are new graduate or experienced nurses transitioning to perioperative nursing practice. Learners are hired directly into a service-line and assigned a primary preceptor narrowing the focus to several surgical subspecialties. The content is divided into 5 five phases of care (See Figure 2). These phases of care, or Entrustable Professional Activities (EPAs) are clusters of interconnected competencies that require the learner to possess knowledge, skill and attitude and apply these within context related to the profession.1,2 High reliability organization concepts, teamwork skills, and patient safety initiatives are integrated throughout the program.
Each phase offers multiple learning modalities including: on-line learning modules, interactive didactic sessions, guest speakers, skills practice, observations in the clinical environment, simulations that increase in complexity, and application of skills within context in the clinical environment with a preceptor. Each phase culminates with a milestone check during a simulation to identify performance gaps. The simulations are designed using the SMARTER approach with clearly defined expected actions and embedded “triggers” within the scenario script.3
The program is further supported by trained preceptors, celebrations of milestones, and dedicated and protected time to reflect, set goals, and evaluate performance with managers, preceptors, and educators.
Observation / Evaluation
The program is evaluated at four levels focused on fiscal and learner outcomes. The following data is tracked to document return on investment: length of orientation, retention rate, and costs. In the pilot program, 7 out of 9 orientees completed orientation in 7 months with a 90% retention rate compared to an average of 12-month orientation and a 57% retention rate in the previous cohort. To evaluate learners’ self-efficacy, the validated Casey-Fink Graduate Nurse Experience Survey instrument is utilized. 100% of RNs from the pilot program agreed or strongly agreed with the following statement from the Casey-Fink Survey: I feel prepared to complete my job responsibilities. Additionally, learners are evaluated and given feedback during milestone checks in simulation and by preceptors in the actual clinical environment.
Discussion
In August 2015, the first group of 10 learners began the pilot program. Feedback is that simulation experiences and milestone checks help learners identify performance gaps and assist preceptors with goal setting during the preceptorship. Further evaluation data from two full cycles will be available by IPSSW2016. The collaborative design process can be utilized by simulation practitioners to create programmatic solutions at their home institutions.